Optical Illusions and 12-Lead ECGs: How First Impressions Can Mislead
ECG Weekly Workout with Dr. Amal Mattu
HPI
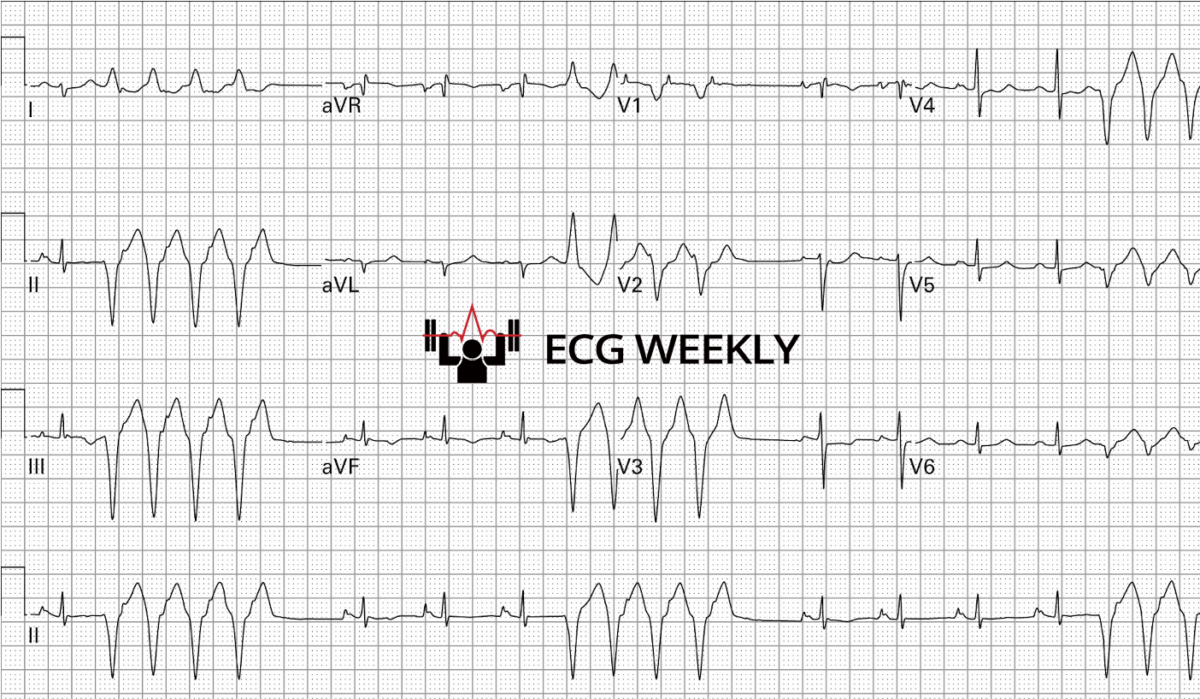
A 42-year-old woman presents to the emergency department with chest pain, shortness of breath, and palpitations. Her blood pressure and mental status are noted to be normal. The following ECG is obtained:
Before watching this week’s workout, carefully review the ECG and consider the following:
-
- What is the most likely diagnosis?
- What treatment does this patient need?
Video
Case Summary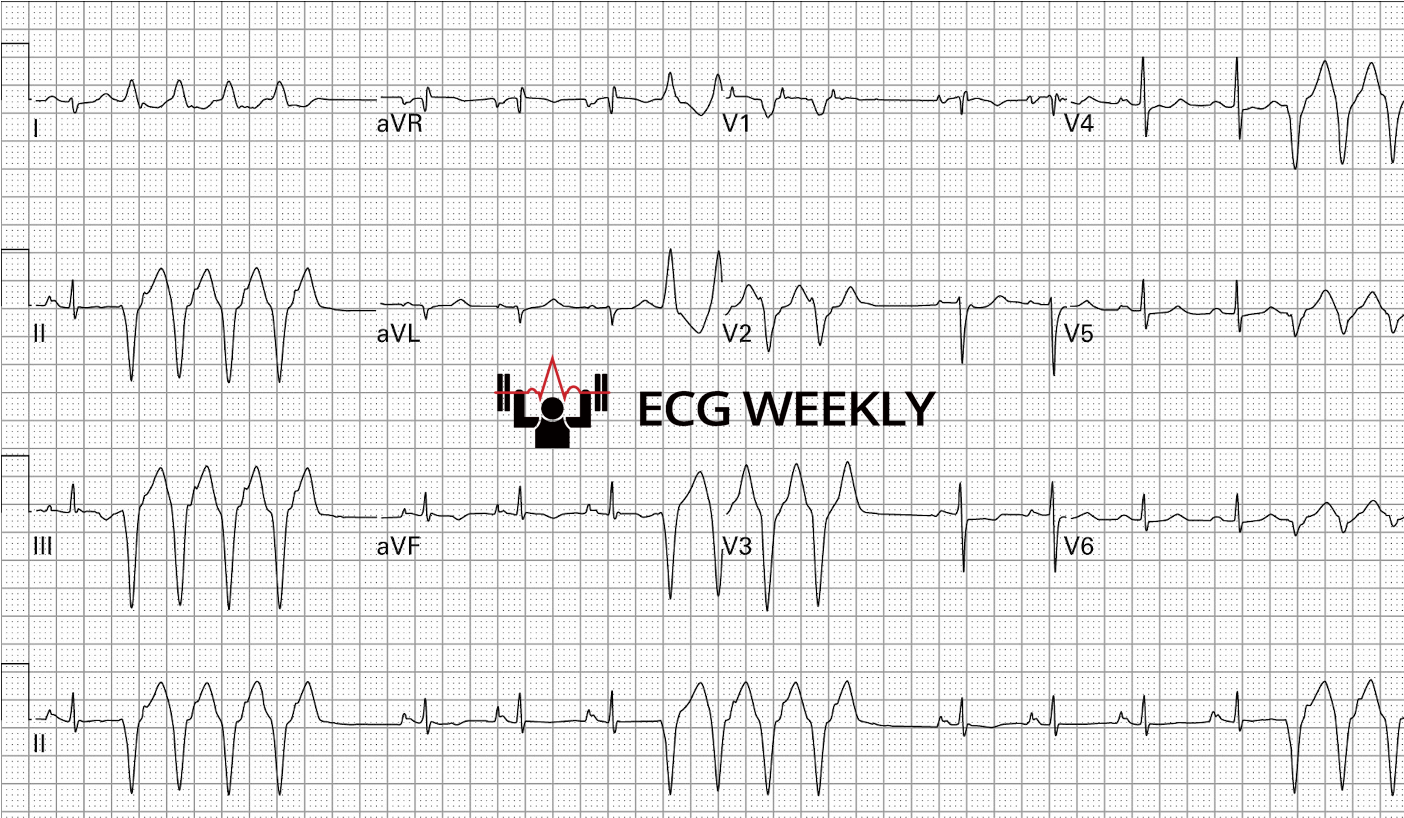
42-year-old woman with chest pressure that occasionally felt “sharp,” accompanying shortness of breath and palpitations. Initial 12-lead ECG showed sinus rhythm in the 90s punctuated by brief runs of wide-complex tachycardia (~170 bpm) consistent with non-sustained ventricular tachycardia (NSVT). Careful stepwise analysis revealed right-axis deviation and T-wave inversions in both inferior and anteroseptal leads, ultimately leading to the diagnosis of acute pulmonary embolism (PE).
Key Teaching Points
- Use a systematic ECG approach every time (rate → rhythm → axis → intervals → ischemia/infarction).
- Even when something dramatic leaps out (e.g., NSVT, obvious STEMI), taking 15–20 seconds to run the checklist prevents missed diagnoses.
- Right-axis deviation plus simultaneous T-wave inversions in inferior and anteroseptal leads strongly suggests PE.
- This pattern is far more common and predictive than the classic “S1Q3T3” (not sensitive or specific).
- Remember your differential diagnosis for right axis deviation.
- Remember your differential diagnosis for T wave inversions.
- Remember the key ECG findings in acute pulmonary embolism.
- Never treat the strip in isolation: NSVT demands a search for the underlying precipitant; anti-arrhythmic suppression alone (lidocaine, amiodarone, procainamide) can mask but not solve the root problem and may worsen outcomes.
- Beta-blockers are the preferred pharmacologic option when NSVT is driven by adrenergic surge, but definitive management hinges on correcting the underlying trigger—in this case, anticoagulation for PE.
- Remember the perceptual trap: Like optical illusions, ECGs can mislead if you fixate on a single striking feature. Step back, view the entire tracing, and correlate clinically. If you have time, don’t settle for your initial impression…look at the whole picture!
Final Take-Home Point
A disciplined, stepwise ECG review can transform a distracting run of NSVT into a lifesaving recognition of pulmonary embolism. Remember your stepwise approach and differentials. Treat the patient, not just the rhythm!