Recent University of Maryland Medical Center Cases (Part II)
UMEM Potpourri ECG Cases with Dr. Amal Mattu
HPI
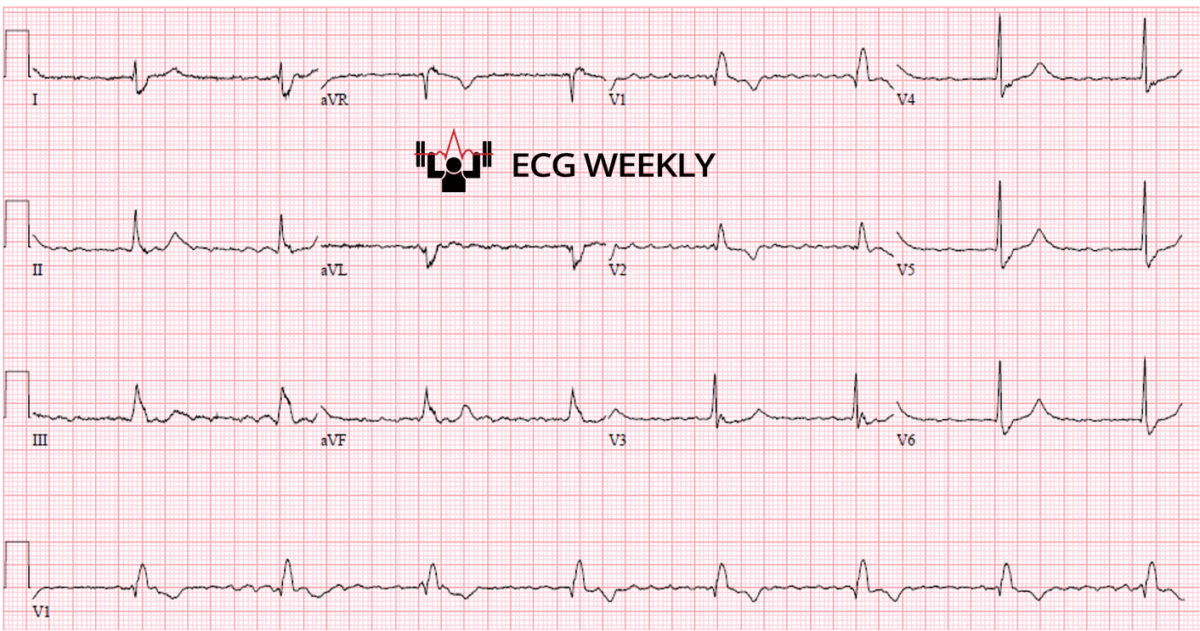
A 72-year-old woman presents to the emergency department with lightheadedness and near-syncope. The following ECG is obtained on arrival:
Before watching this week’s workout, carefully review the ECG and consider the following:
-
- What is the atrial rhythm?
- What is the ventricular rate and rhythm?
- What is your diagnosis?
Video
Kudos
Thanks to the University of Maryland Medical Center's Department of Emergency Medicine for sharing their cases for this series.This week, we continue with part 2 in our series of interesting recent cases from the University of Maryland Medical Center. This episode continues from the previous week with more instructive ECG cases from the emergency department, emphasizing key ECG interpretation pearls and diagnostic challenges.
Case 6: Wellens Syndrome (Biphasic T wave Pattern)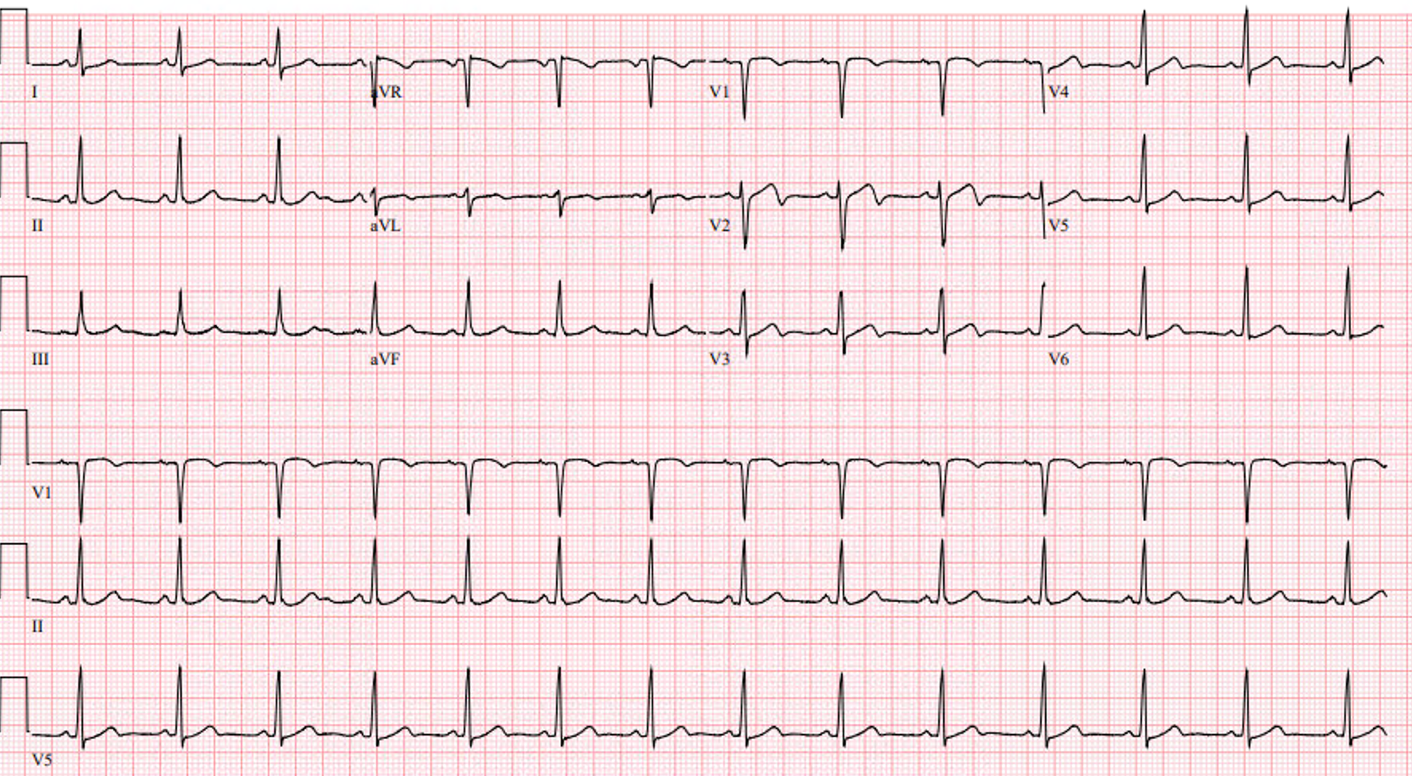
- Patient: 35-year-old woman presenting with concerning chest pain, now resolved.
- Key ECG Finding: Biphasic T-waves in leads V2, V3, possibly V4 without significant ST-segment changes.
- Diagnosis: Wellens syndrome indicating critical proximal LAD stenosis.
- Key Points:
- Two patterns of Wellens waves: deeply inverted or biphasic T waves in mid-precordial leads.
- Wellens predicts critical (subacute) LAD stenosis despite resolved pain.
- Often misinterpreted by computers as “non-specific,” but clinically significant.
Case 6c: Wellens Waves Mimic (Early Repolarization Variant)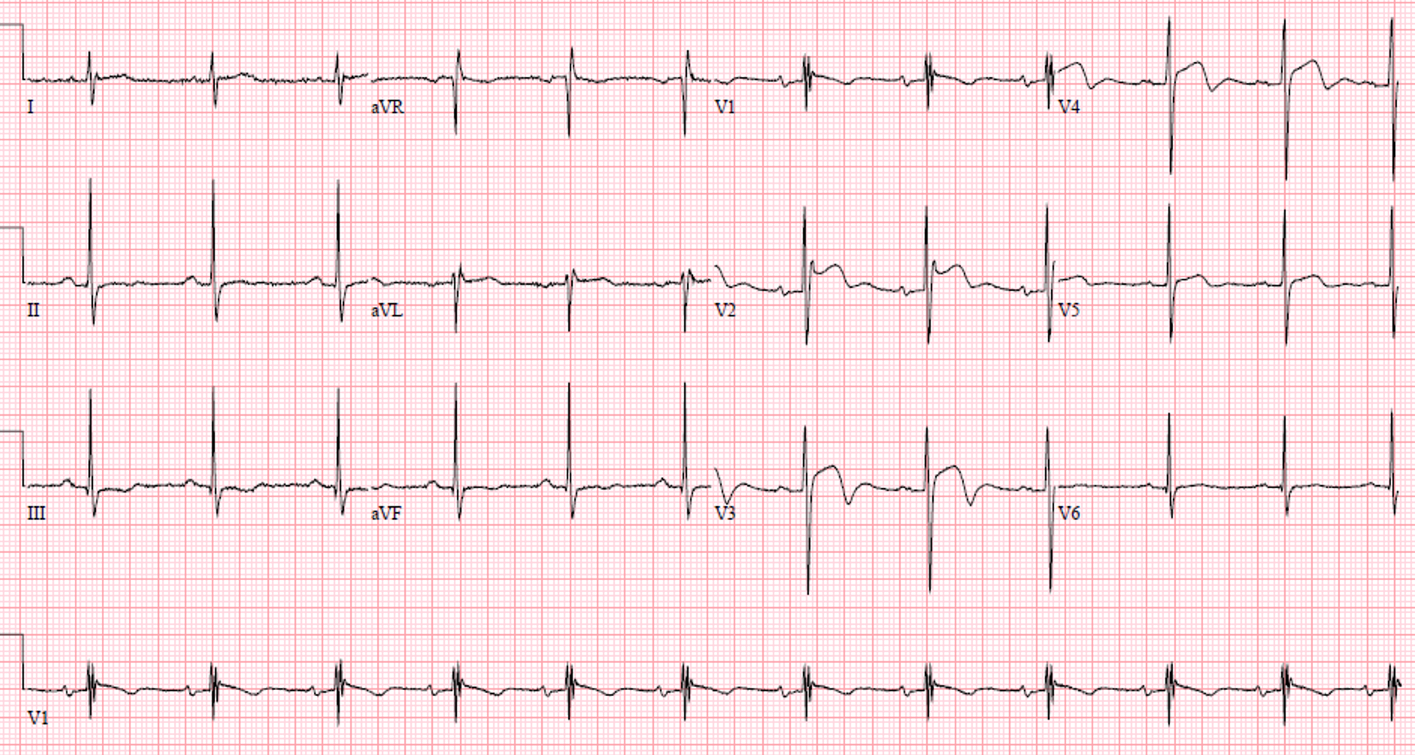
- Patient: Typically young men of African or Caribbean descent.
- Key ECG Finding: High voltage, J wave followed by concave upward ST segment, then sharp drop into T wave inversion.
- Diagnosis: Early repolarization variant (typically benign condition).
- Key Points:
- Distinguishable from true Wellens by presence of J wave, concave upward morphology before T wave inversion.
- True Wellens lacks J waves, showing abrupt straight or biphasic T wave inversion without preceding concave ST morphology.
- Important to distinguish as benign to avoid unnecessary interventions.
Case 7: Complete Heart Block with Ventricular Escape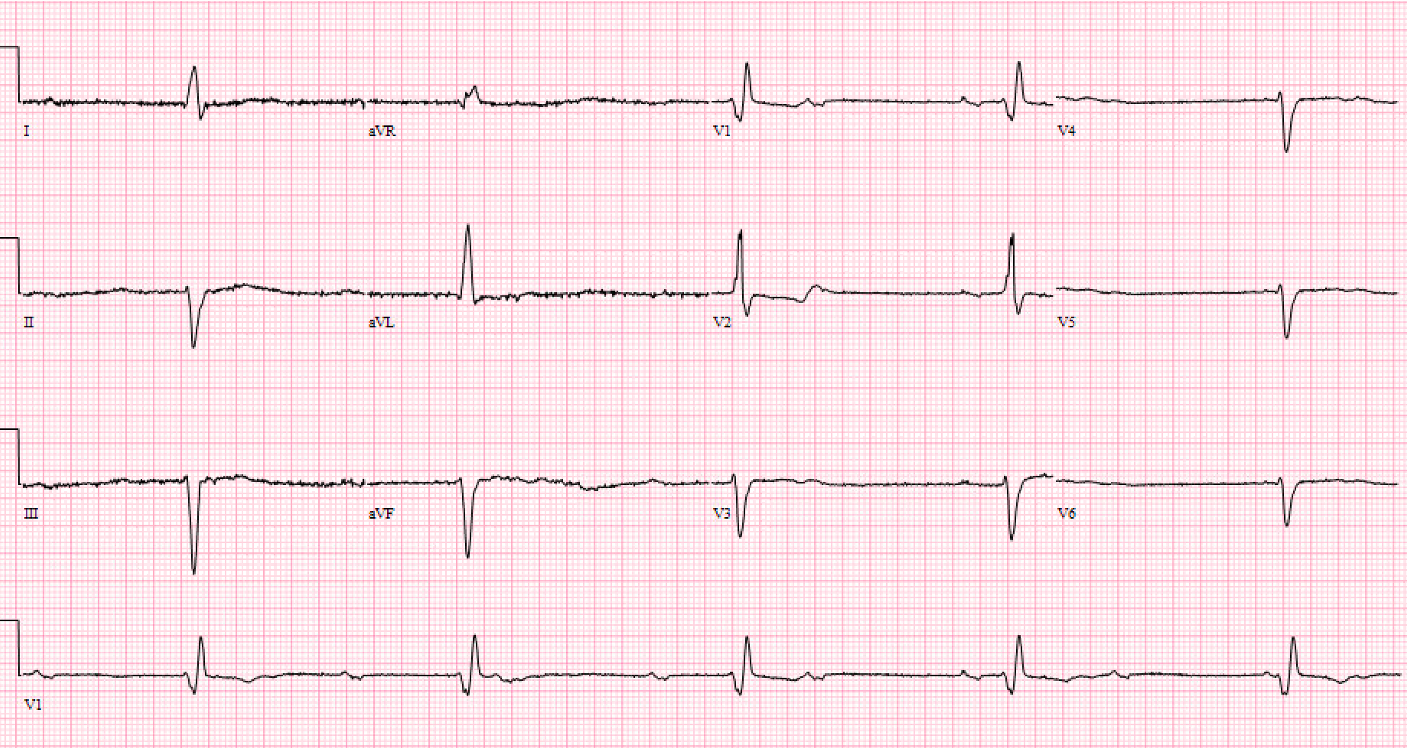
- Patient: 82-year-old man with syncope.
- Key ECG Findings:
- Atrial (P wave) rhythm and ventricular (QRS) rhythm dissociated.
- Regular, wide-complex ventricular escape rhythm at a slow rate (20-40 bpm).
- Diagnosis: Complete heart block with ventricular escape rhythm.
- Key Points:
- Complete heart block always shows regular escape rhythm independent of atrial activity.
- Slow and wide escape rhythms typically originate from ventricles.
- Important to distinguish from Mobitz blocks (irregular rhythms).
Case 8: CHB with Junctional Escape (and Underlying Inferior/Posterior MI)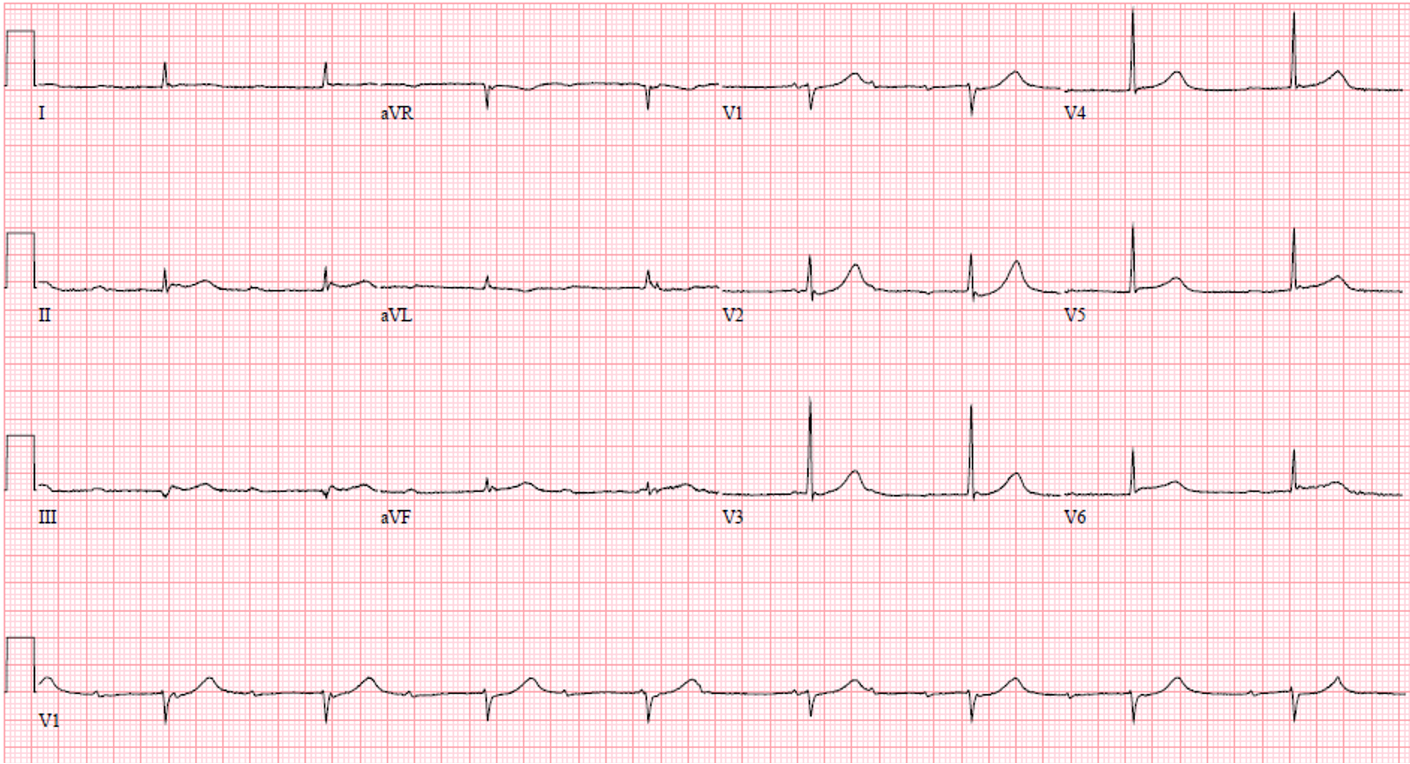
- Patient: 83-year-old with lightheadedness.
- Key ECG Findings:
- Regular narrow-complex ventricular escape rhythm (40-60 bpm).
- Independent sinus tachycardia with dissociated P waves (electrocardiographic “polyuria”).
- ST segment elevation inferiorly and prominent R-waves in V2/V3 suggesting posterior MI.
- Diagnosis: Complete heart block, junctional escape rhythm, likely secondary to acute inferior/posterior MI.
- Key Points:
- Regular narrow escape rhythms typically indicate junctional origin.
- Inferior MI commonly associated with conduction disturbances (e.g., complete heart block).
Case 9: Atrial Fibrillation with CHB & Junctional Escape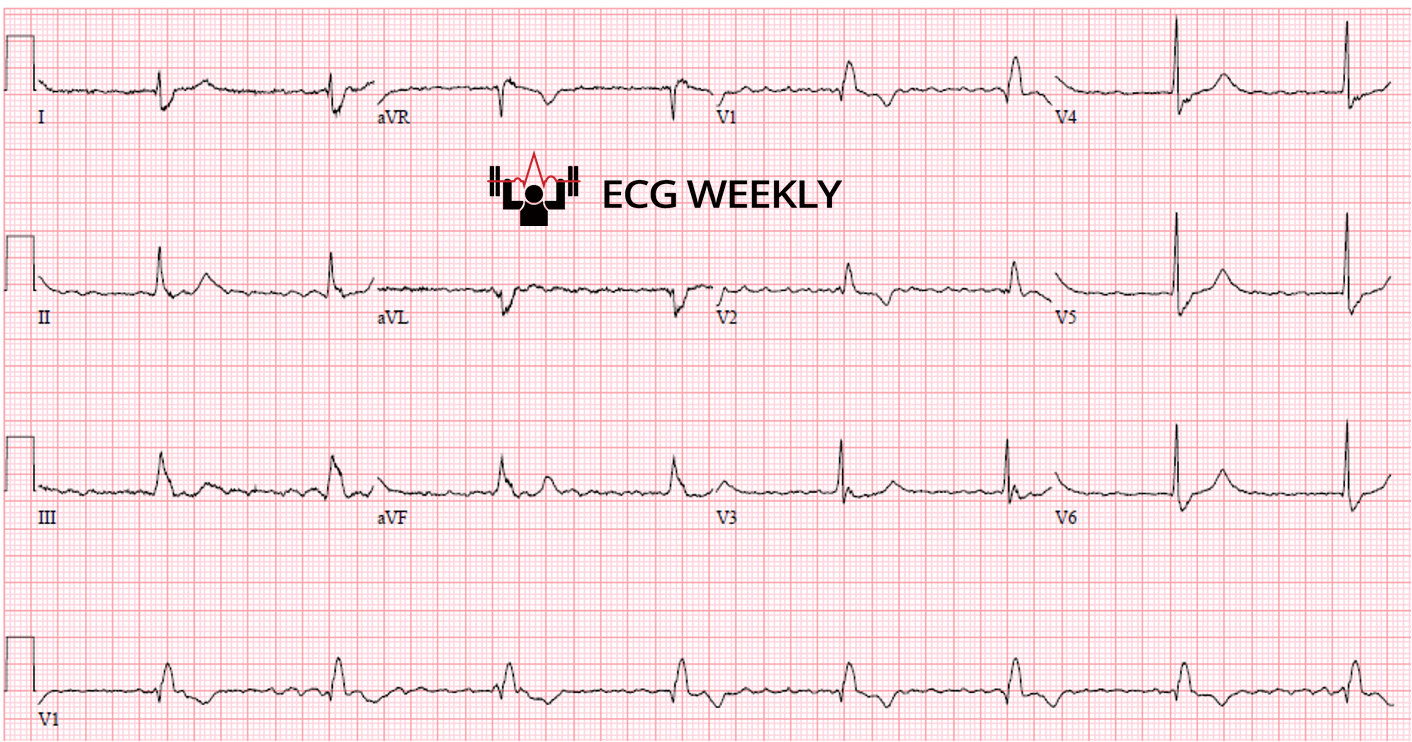
- Patient: 72-year-old woman with lightheadedness.
- Key ECG Findings:
- Irregular fibrillatory atrial activity (atrial fibrillation).
- Unexpectedly regular ventricular rhythm with widened QRS complexes (right bundle branch block pattern), rate ~50 bpm.
- Diagnosis: Atrial fibrillation with complete heart block and junctional escape rhythm, secondary to calcium channel blocker toxicity.
- Key Points:
- Regular ventricular response in atrial fibrillation implies complete heart block.
- Junctional escape rhythm usually narrow; wide if bundle branch block present.
- Commonly seen in medication overdose (beta-blockers, calcium channel blockers, digoxin historically).
Final Take Home Points:
- Wellens waves require urgent cardiology evaluation (proximal LAD stenosis).
- Distinguish Wellens from benign early repolarization patterns (J wave morphology, high voltages, patient demographics).
- Complete heart block characterized by AV dissociation and regular escape rhythms (junctional 40-60 bpm narrow, ventricular 20-40 bpm wide).
- Atrial fibrillation with a regular ventricular response strongly suggests complete heart block and potential medication toxicity.
This week Dr. Mattu emphasized precise ECG interpretation, recognizing subtle but critical findings, and maintaining skepticism toward computerized ECG interpretations to ensure appropriate patient management. We continue next week with the last part of our interesting cases from the University of Maryland ED, stay tuned!