In the Era of High-Sensitivity Troponin, Does Unstable Angina Still Exist?
Emergency Cardiology Literature Review & Updates with Dr. Amal Mattu
HPI
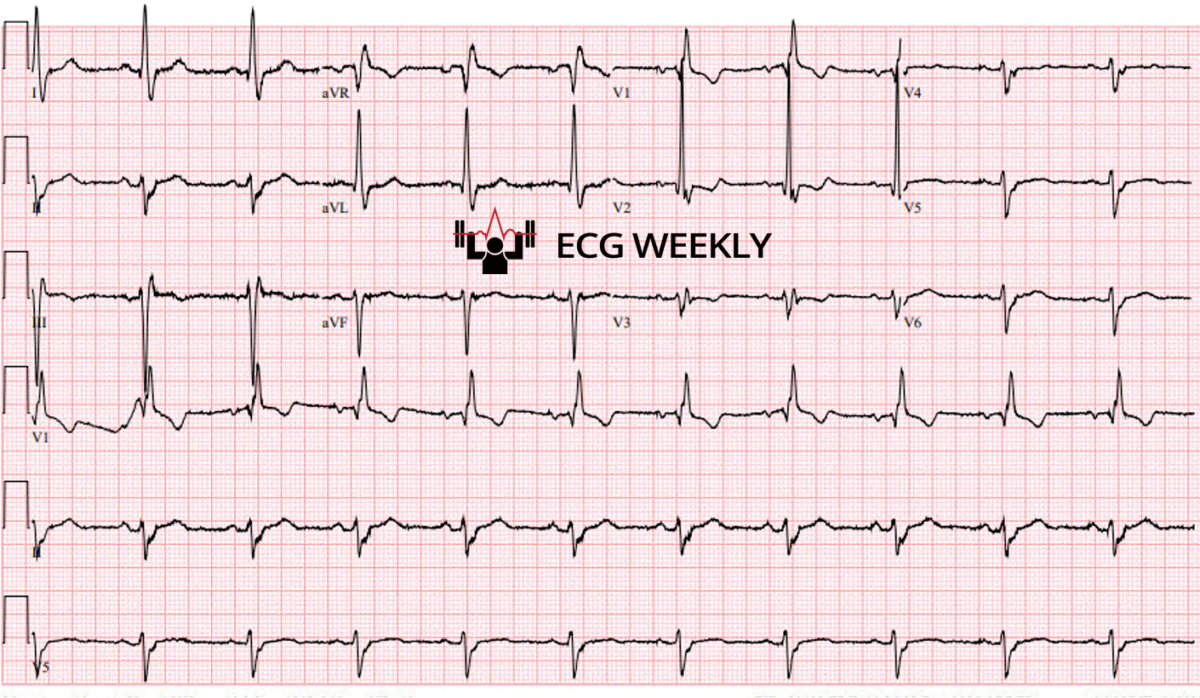
A 92-year-old man presents to the emergency department with gradually worsening dyspnea on exertion that has progressed to exertional chest “fullness”. He is asymptomatic on arrival with normal vitals. The following arrival ECG is obtained and noted to have a bifascicular block that is unchanged from prior. High-sensitivity troponin values are within normal limits and unchanged with repeat testing, meeting a common “rule-out” pathway for ACS.
Before watching this week’s workout, review the arrival ECG carefully and consider:
-
- Based on this history, ECG context, and non-dynamic hs-troponins, has ACS been ruled out? Would you discharge this patient?
- What specific features in the history should override a protocol-based “rule-out” and push you toward further testing rather than discharge?
- If you are not discharging, what is the most defensible next step: observation with serial ECGs, stress testing strategy, coronary CTA, or cardiology consultation for invasive evaluation?
Video
Kudos
Thanks to Dr. Garrett Ghent for sharing his case for this week’s workout.This week, Dr. Mattu shifts from a pure ECG focus to a literature-driven pitfall he is seeing clinically and in active medicolegal work: over-reliance on high-sensitivity troponin protocols to “rule out ACS”, while under-weighting history and ECG interpretation beyond “STEMI vs no STEMI.”
Case 1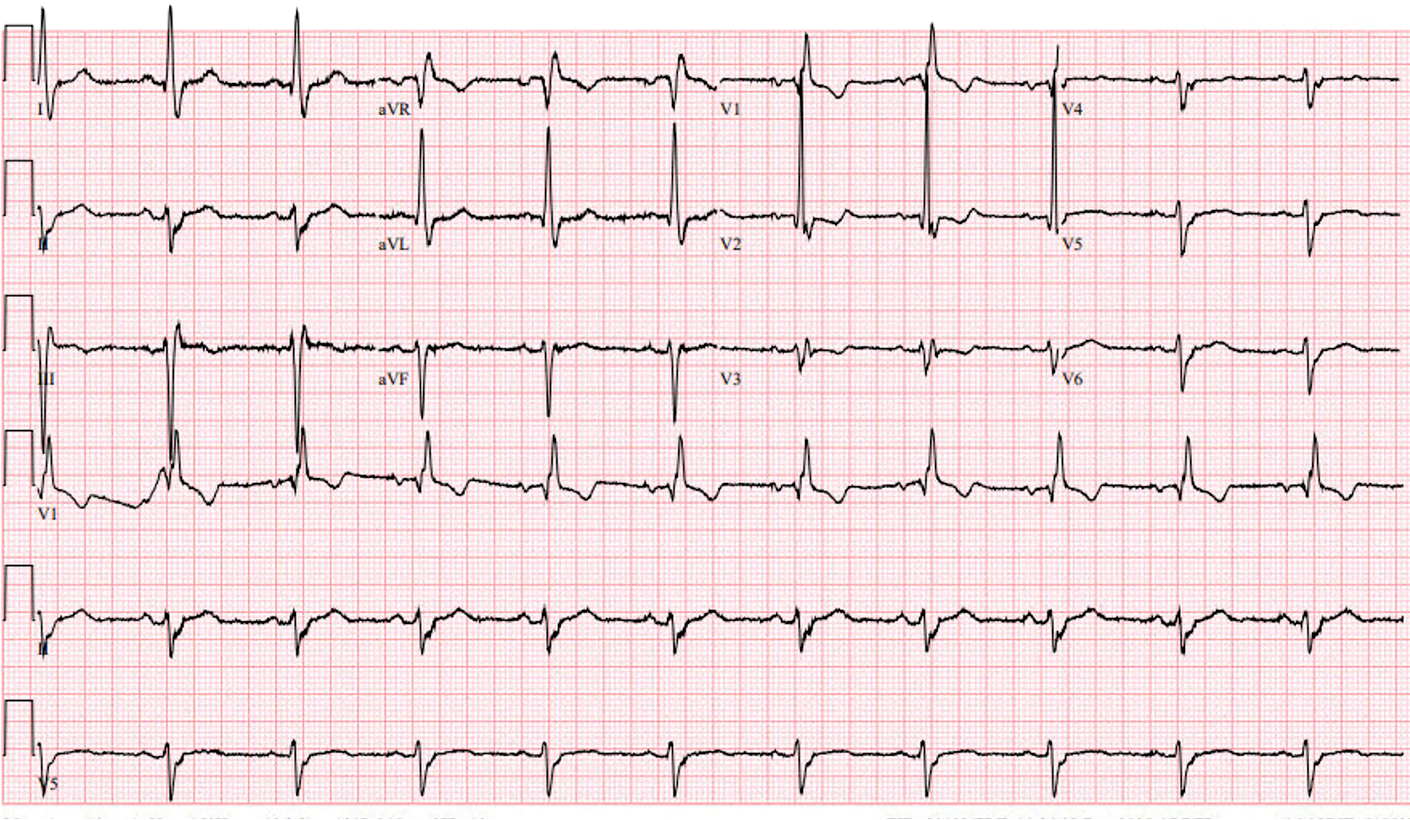
A 92-year-old man presents with gradually worsening dyspnea on exertion that has evolved into exertional chest “fullness.” He avoids calling it “pain,” which Dr. Mattu highlights as a common history trap if clinicians only ask about “pain.” He has multiple cardiac risk factors and is asymptomatic on arrival with normal vitals and exam.
ECG shows sinus rhythm with a right bundle branch block plus left anterior fascicular block (bifascicular block), similar to prior, and no clearly new ischemic changes. The patient is placed into a commonly referenced high-sensitivity troponin algorithm. His hs-troponin T is 9 at baseline and 9 at a little over 1 hour, meeting an algorithmic “rule-out” pathway despite a concerning exertional symptom complex.
Dr. Mattu’s point: high-sensitivity troponin is highly sensitive for myocyte necrosis, not for ischemia without necrosis. Unstable angina remains a real entity. The treating team does not let a protocol override the clinical picture and proceeds with coronary CTA, then cath. Cath reveals critical coronary disease, including a 99% proximal and mid LAD lesion that is stented, and additional multivessel disease. The team documents the diagnosis as unstable angina.
Case 2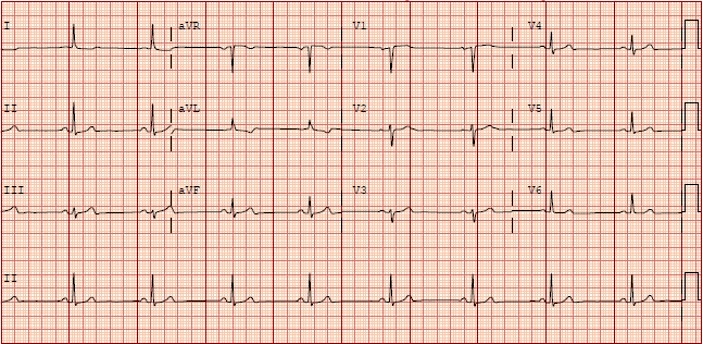
A 70-year-old woman arrives with severe substernal chest aching radiating to both shoulders and elbows, with diaphoresis. Pain began at 7:00 PM and is ongoing on arrival. Initial ECG during active pain is not diagnostic for STEMI, with at most nonspecific findings.
Her hs-troponin is 11, then 13 at about 3 hours after onset (still below the typical female 99th percentile threshold used in many labs). Dr. Mattu emphasizes that some protocols and mindsets would interpret this as a complete ACS rule-out. The team instead recognizes the history as high risk and continues observation.
At about 5.5 hours after onset, symptoms worsen and a repeat ECG shows an acute high lateral STEMI pattern with clear ST elevation in aVL and reciprocal changes. The patient goes emergently to the cath lab. A subsequent troponin returns elevated, and cath shows a 99% distal RCA lesion.
Take-Home Message
Dr. Mattu reiterates that ACS assessment requires integration of history, ECG, and troponins. He explicitly pushes back on the claim that unstable angina is “dead,” citing that contemporary guidelines still include unstable angina within ACS and define it as ischemia without myonecrosis. He references the 2013 Braunwald editorial raising the question of whether unstable angina is becoming obsolete, then contrasts that with current guideline language. He closes with a medicolegal warning and a memorable line: do not let protocol thinking replace your clinical judgment!
Take-Home Points
- High-sensitivity troponin detects myocardial necrosis, not ischemia in the absence of necrosis. A “negative” or non-dynamic hs-troponin does not fully exclude ACS when the clinical story is high risk.
- Unstable angina still exists: ischemia without detectable myonecrosis. Contemporary ACS guidance continues to include unstable angina alongside NSTEMI and STEMI.
- Protocols can be misapplied when they are treated as stand-alone decision makers. History and ECG interpretation must remain active inputs, not afterthoughts. “Only a dope relies purely on a trop!”.
- Serial reassessment matters. If the patient remains symptomatic, worsens, or your concern persists, repeat ECGs and continued observation can be lifesaving even after an early “rule-out” time point.
- ECG review is more than “STEMI vs no STEMI.” The ECG is part of risk assessment and should be scrutinized for ischemia, baseline confounders, and change over time.
References:
- Rao, S, O’Donoghue, M, Ruel, M. et al. 2025 ACC/AHA/ACEP/NAEMSP/SCAI Guideline for the Management of Patients With Acute Coronary Syndromes: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. JACC. Feb 27, 2025. PMID: 40014670
- Januzzi JL Jr, Mahler SA, Christenson RH, et al. Recommendations for Institutions Transitioning to High-Sensitivity Troponin Testing: JACC Scientific Expert Panel. J Am Coll Cardiol. 2019 Mar 12;73(9):1059-1077. Epub 2019 Feb 21. PMID: 30798981
- Braunwald E, Morrow DA. Unstable angina: is it time for a requiem? Circulation. 2013 Jun 18;127(24):2452-7. PMID: 23775194