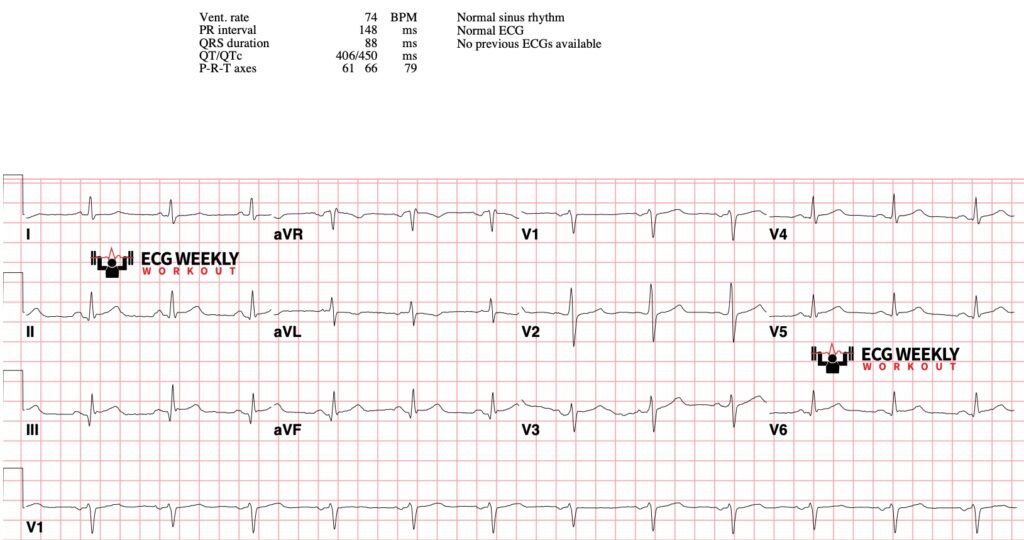
Key Points
- Clinical Context: Abnormal ECG findings in emergent settings must always be interpreted within the clinical context. Not all abnormalities represent life-threatening conditions, while severe conditions may present subtly or even normally.
- Serial Monitoring: Serial ECGs, additional diagnostic evaluations, and close clinical observation are critical in high-risk patients to ensure significant diagnoses are not missed.
- Documentation: Clearly document both abnormal and normal findings, emphasizing relevance to clinical symptoms and decision making.
- Customized Interpretation: Tailor your ECG interpretation to the clinical scenario and presenting symptoms for optimal management and documentation of your medical decision making.
Abnormal STAT ECG Findings:
Heart Rate:
- Tachycardia (>100 bpm Adults; Pediatrics vary by age):
- Evaluate for sinus tachycardia (fever, pain, hypovolemia) versus pathologic arrhythmias (SVT, VT, AFib).
- Bradycardia (<60 bpm Adults; Pediatrics vary by age):
- Assess for symptomatic bradycardia, AV blocks, medication effects, or electrolyte abnormalities.
- Pediatric Considerations:
- Recognize age-dependent normal heart rates to avoid misinterpretation:
- Neonates (0-1 month): 90-180 bpm
- Infants (1 month-1 year): 100-160 bpm
- Toddlers (1-3 years): 90-150 bpm
- Preschoolers (3-5 years): 80-140 bpm
- School-aged (6-12 years): 70-120 bpm
- Adolescents (13-18 years): 60-100 bpm
- QTc abnormalities in pediatrics carry similar arrhythmogenic risks as adults and require attention
- Recognize age-dependent normal heart rates to avoid misinterpretation:
Rhythm:
- Irregular Rhythm:
- Consider atrial fibrillation/flutter; crucial to document clearly in stroke evaluations.
- Ectopy:
- Evaluate significance of premature atrial or ventricular complexes, considering clinical context.
Axis Deviation:
- Left Axis Deviation (LAD):
- Suggestive of LVH, left anterior fascicular block, or inferior MI.
- Right Axis Deviation (RAD):
- Indicates right ventricular strain (PE, COPD, pulmonary hypertension), sodium channel blocker toxicity, or hyperkalemia.
Intervals:
- PR Interval:
- Prolonged (>200 ms): Indicates AV block or conduction delay; critical in syncope workup.
- Short (<120 ms): Suggests pre-excitation syndromes (WPW).
- QRS Duration:
- Wide (>120 ms): Suggests bundle branch blocks, ventricular rhythms, hyperkalemia, sodium-channel blocker toxicity.
- QTc Interval:
- Prolonged (>500 ms): Significant risk for Torsades de Pointes.
- Short (<350 ms): Risk factor for ventricular arrhythmias and sudden cardiac death.
Waveform Morphology:
- Q Waves:
- Pathologic: >1 small box wide or >1/3 height of R wave, indicating prior MI.
- Poor R Wave Progression:
- Suggests prior anterior MI or cardiomyopathy.
ST Segment:
- Elevation: Highly suggestive of acute occlusion myocardial infarction (STEMI); immediate intervention needed.
- Depression: Indicates ischemia; clinical correlation required. Depression in V1-V3 may be from Posterior STEMI.
T Waves:
- Inversion: May represent ischemia, especially if dynamic or correlating with symptoms.
- Peaked T Waves: Suggestive of acute hyperkalemia; absence reassuring in ESRD patients.
Common Pitfalls in Abnormal ECG Interpretation:
- Hidden Ischemia:
- Normal/subtle ECG changes do not rule out ischemia. Maintain high suspicion and perform serial evaluations.
- Lead Misplacement:
- Incorrect placement can mimic or obscure true ECG abnormalities.
- Normal Variants:
- Recognize benign ECG patterns (e.g., early repolarization, juvenile T-wave inversions) to prevent misdiagnosis.
Key Clinical Scenarios & Documentation Tips:
- Chest Pain:
- Clearly document presence or absence of STEMI/equivalent criteria.
- Stroke Evaluation:
- Confirm/document absence or presence of atrial fibrillation/flutter.
- Dyspnea:
- Clearly document right heart strain features suggestive of PE.
- Syncope:
- Document rhythm disturbances, conduction abnormalities, prolonged intervals, epsilon waves, or ischemic changes suggestive of a cardiac cause.
- End-Stage Renal Disease:
- Document T-wave morphology clearly to evaluate hyperkalemia risks.
KEY CLINICAL PEARLS:
- Always personally review ECGs; do not rely solely on computer interpretations or trust "Normal ECG" interpretations. Computers will miss early signs of ischemia and other life threatening conditions.
- Integrate ECG abnormalities into the broader clinical picture to guide management effectively.
- Lead Misplacement Pitfalls:
- Precordial Leads: V1 and V2 placed too high can mimic anterior MI or RBBB.
- Limb Leads: Reversed leads can alter the axis and create false pathology.
- Normal Variants to Recognize:
- Early Repolarization: Common in young, healthy people; can look like ST elevation but is harmless.
- Benign T Wave Inversion: Often seen in leads III and aVF, especially in young females.
- Watch for Hidden Ischemia:
- A normal ECG doesn't rule out ischemia. Consider serial ECGs and further testing if clinical suspicion is high.
Related Topics & Recommendations:


