A Decade of ECG Gems: The Final 5 Favorite Cases
ECG Weekly Workout with Dr. Amal Mattu
HPI
A 50-year-old woman presents with palpitations. She reports symptoms of an upper respiratory infection and has a low grade fever. The following ECG is obtained:
Before watching this week’s workout, closely examine the ECG and ask yourself:
-
- What is the rhythm?
- What is the most likely diagnosis?
- What antiarrhythmic medications would you want to avoid in this case?
Video
Kudos
Thanks to Drs. Anver Sethwala, Ahmed Alkhaisey, Gaser Ahmed, Justin Cormack, Nikhil Tambe, Sanjay Mehta, Salem AlGhamdi, & Rudi Beckers for sharing their cases this week! Also, a huge thank you to all the wonderful contributors and subscribers that have been along for ECG Weekly’s journey over the past 10 years!Continuing the celebration of ten years (522 consecutive weeks) of ECG Weekly, Dr. Mattu presents his top five favorite ECG cases from the past decade. These cases showcase rare or easily missed diagnoses, each emphasizing the importance of a methodical, thorough approach to ECG interpretation. In addition, Dr. Mattu shares an upcoming conference announcement and expresses gratitude to the ECG Weekly community for contributing so many educational cases over the years.
Top 5 Cases of the Decade
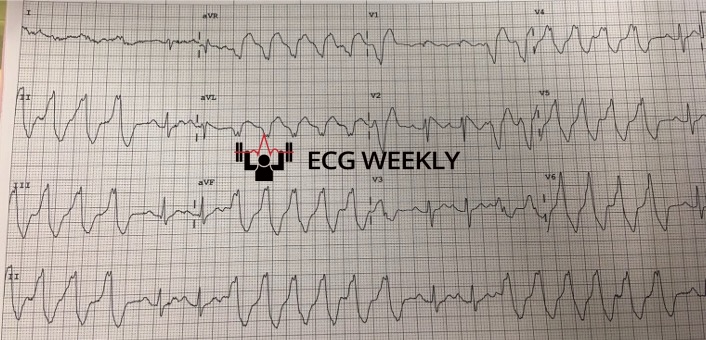 Case #5: Brugada Hiding in Between NSVT Runs (December 17, 2018)
Case #5: Brugada Hiding in Between NSVT Runs (December 17, 2018)
Key Highlights:
- Presentation: A 50-year-old with palpitations, low-grade fever, and runs of nonsustained ventricular tachycardia (NSVT).
- Surprise Finding: On close inspection of the beats between the NSVT runs, the patient has Brugada Syndrome (characteristic coved ST elevations in V1–V2).
- Take-Home Points:
- Avoid Sodium Channel Blockers (e.g., procainamide, amiodarone) in suspected Brugada to prevent malignant arrhythmias.
- Always inspect the “quiet” parts of the ECG; the biggest clue might lie in seemingly unremarkable beats. Be thorough in your evaluation.
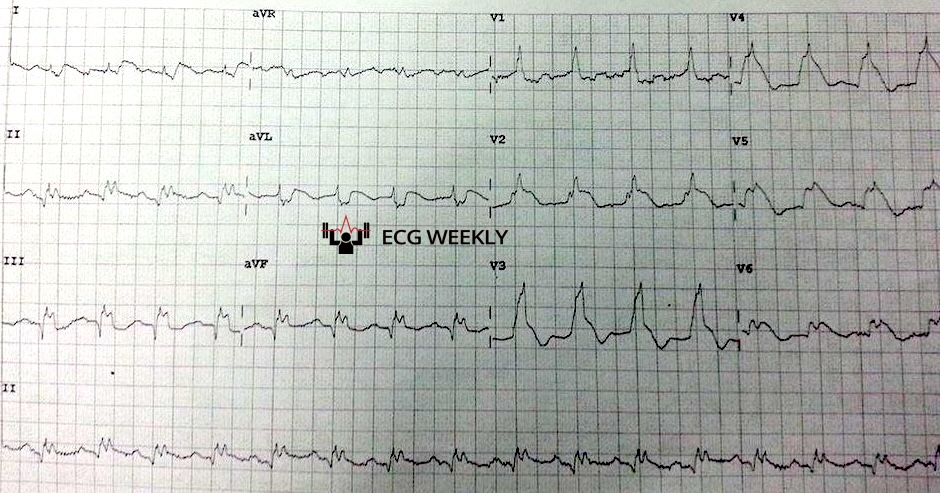
 Case #4: Potential Side Effect of Adenosine
Case #4: Potential Side Effect of Adenosine
- May 20, 2024 – SVT Treated with Adenosine → AF + WPW
- Patient developed rapid atrial fibrillation with WPW conduction after receiving adenosine for presumed SVT.
- Key Point: Adenosine can unmask or induce AF in patients with undiagnosed WPW, necessitating prompt cardioversion if unstable.
- December 6, 2021 – Pregnant Patient with SVT → AF + WPW
- Similarly, a 25-year-old at 39 weeks gestation received adenosine for SVT and developed AF with WPW.
- Take-Home Points:
- No antiarrhythmic is entirely “safe”!
- Adenosine may trigger AF, which becomes dangerous if underlying WPW is present. Adenosine has been reported to cause SVT to turn into AF in up to 12% of cases.
- Be prepared to cardiovert when using any antiarrhythmic; always have defibrillation on standby.
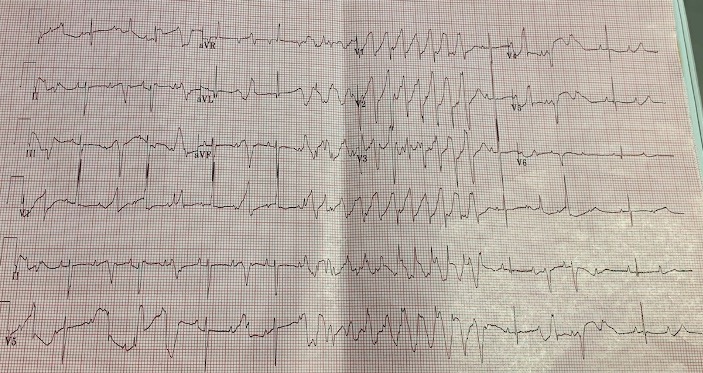
 Case #3: Spiked Helmet Sign (December 21, 2015)
Case #3: Spiked Helmet Sign (December 21, 2015)
- Presentation: A 64-year-old with chest pain radiating to the neck, neurologic symptoms, and a bizarre-looking QRS complex in V2 that resembled a spiked helmet.
- Outcome: The patient arrested (PEA) shortly thereafter.
- Take-Home Points:
- This unusual spiked helmet sign on ECG is consistently associated with critical illness and high risk of imminent cardiac arrest—an alarm for expedited diagnosis and intervention.
- Cause of the morphology is uncertain, upward shift of the baseline begins prior to the QRS complex.
- Suggests intra-abdominal pathology if present in limb leads. Suggests intra-thoracic pathology if present in the precordial leads.
 Case #2: T-Wave Alternans in a Pediatric Patient (December 30, 2019)
Case #2: T-Wave Alternans in a Pediatric Patient (December 30, 2019)
- Presentation: An infant with persistent GI illness and an ECG demonstrating long QT and T-wave alternans (amplitude changes in consecutive T-waves).
- Take-Home Points:
- T-wave alternans (beat to beat variation in size or shape of the T wave) is a red flag for impending Torsades de Pointes or other malignant arrhythmias.
- Recognize it promptly, treat the underlying cause, and administer IV magnesium as indicated.
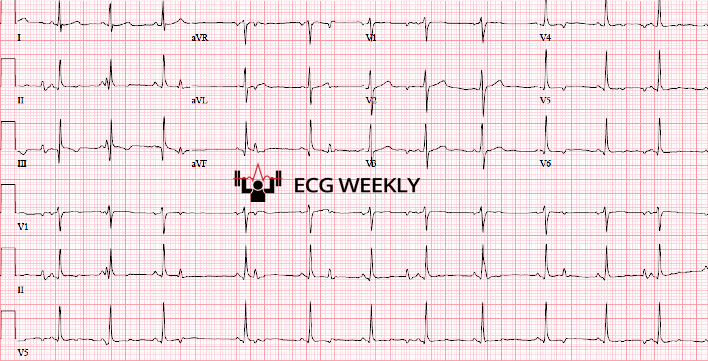 Case #1: Atrial Parasystole (August 2, 2021)
Case #1: Atrial Parasystole (August 2, 2021)
- Presentation: A 17-year-old with stable palpitations and an ECG revealing two distinct P-wave morphologies, each pacing the atria independently.
- Significance:
- Atrial parasystole is rare in routine practice but is a fascinating example of two atrial foci firing concurrently with no mutual suppression.
- Underlines the importance of carefully examining P-wave morphology and regularity.
Final Thoughts & Honorable Mentions
- Other noteworthy, “honorable mention” cases from the past decade include: Hypercalcemia mimicking STEMI, Lewis lead, pulse-tapping artifact, crochetage pattern, isorhythmic AV dissociation, and intermittent hidden WPW.
- Message of Thanks: Dr. Mattu expresses gratitude for the community’s involvement and looks forward to another decade of amazing case submissions and ECG discoveries.
Stay tuned for more cutting-edge ECG discussions and have a safe, happy New Year!



