Not Cerebral T Waves: The Beat-to-Beat Warning You Cannot Miss
ECG Weekly Workout with Dr. Amal Mattu
HPI
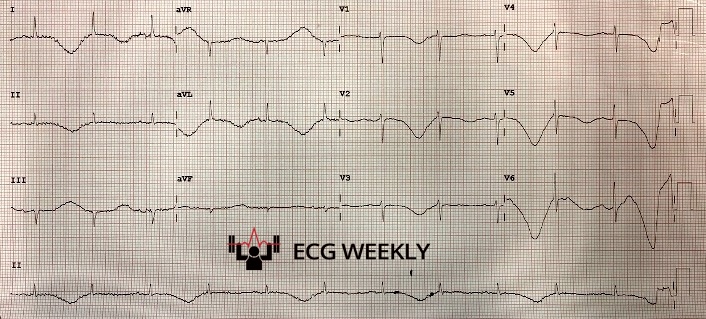
A 71-year-old woman with baseline dementia presents with worsened confusion, nausea, and multiple episodes of vomiting over the past 24 hours. Her vital signs are reasonable and her exam is non-diagnostic. An ECG obtained on arrival shows deep T wave inversions and QT prolongation. Many clinicians would suspect cerebral T waves and immediately send her for head CT. However, another dangerous abnormality present on the ECG is noticed before she develops polymorphic ventricular tachycardia.
Before watching this week’s workout, review the arrival ECG carefully and consider:
-
- What specific T wave finding would make you abandon the “cerebral T wave” diagnosis and prepare for a malignant arrhythmia that could occur in minutes?
- When an altered patient has deep T wave inversions and a long QT, what detail determines whether they need a head CT or immediate arrhythmia-focused interventions?
- What bedside steps stabilize a patient who is slipping in and out of polymorphic VT due to repolarization instability?
Video
Kudos
Thanks to Drs. Aaron Wynn, Salem AlGhamdi, Mike Akkhasian, David Zira, and Jason Roediger for sharing their cases for this week’s workout!Reminder: All ECG Weekly subscribers can get an exclusive discount to Journal Feed and try it out risk free with no obligations here: www.journalfeed.org/ecgweekly.
A 71-year-old woman with baseline dementia presents with 24 hours of worsening confusion and recent vomiting. Her vitals look reasonable. Broad labs and a 12-lead ECG are obtained. That ECG immediately draws attention with most clinicians focusing on the deep, symmetric T wave inversions and prolonged QT interval. Many would call these “cerebral T waves,” worry about intracranial catastrophe, and send her straight to CT.
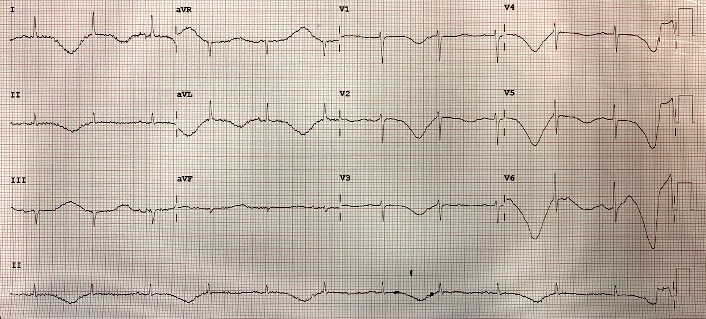
That reflex is understandable given her altered mental status and vomiting. But the key abnormality is not simply the T wave inversion. It is the beat-to-beat alternation in T wave size and morphology. The T wave is inverted on one beat, then flatter on the next, then inverted again: true T wave alternans.
This matters because T-wave alternans is one of the strongest ECG predictors of impending torsade de pointes and sudden cardiac arrest. Minutes later, the patient develops polymorphic ventricular tachycardia consistent with torsade, intermittently self-terminating.
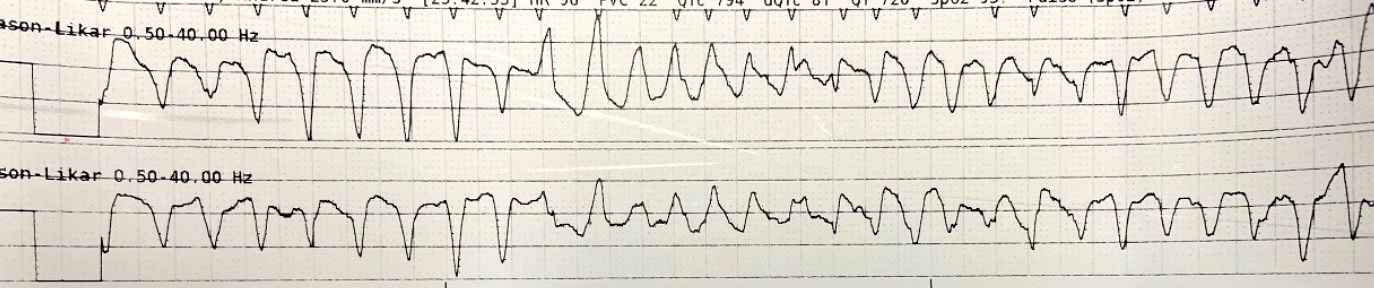 Since the arrhythmia was not sustained, immediate defibrillation was not required. Instead, Dr. Wynn initiated overdrive therapy with isoproterenol to accelerate the heart rate. Increasing the rate to around 120 bpm shortens the QT interval and suppresses torsade. Electrolyte evaluation showed hypokalemia and hypomagnesemia, likely from vomiting, and both were aggressively corrected. After rate acceleration and electrolyte repletion, torsade episodes cease.
Since the arrhythmia was not sustained, immediate defibrillation was not required. Instead, Dr. Wynn initiated overdrive therapy with isoproterenol to accelerate the heart rate. Increasing the rate to around 120 bpm shortens the QT interval and suppresses torsade. Electrolyte evaluation showed hypokalemia and hypomagnesemia, likely from vomiting, and both were aggressively corrected. After rate acceleration and electrolyte repletion, torsade episodes cease.
Dr. Mattu then reviews earlier cases showing identical physiology: marked QT prolongation with true alternation in T wave amplitude prior to torsade. He stresses that computer algorithms never detect T wave alternans. It must be recognized by the clinician and taken seriously. A prolonged QT alone is common. QT prolongation with alternans is a high-risk marker for cardiac arrest within minutes.
He also reviews R-on-T phenomenon as another potent torsade trigger. He demonstrates how incorrect pacer sensing can shock on a T wave and precipitate VF. Anytime pacing spikes appear on T waves, the synchronization must be confirmed or corrected immediately.
The episode closes with a broader lesson: clinicians consistently under-value the T wave. Dr. Mattu emphasizes the enormous diagnostic and prognostic information embedded in T wave morphology: hyperacute T waves, de Winter pattern, reperfusion changes, PE patterns, ARVC, Wellens waves, pseudo-Wellens waves, hyperkalemia, hypokalemia, Himalayan patterns, cerebral T waves, and most urgent in this case — T wave alternans. The moral of this story is clear: a prolonged QT with beat-to-beat T wave alternans means torsade is imminent. Fix electrolytes now, accelerate the rate, start magnesium, and be prepared for defibrillation.
Key Teaching Points:
- T wave alternans (beat-to-beat variation in size or shape of T wave) plus prolonged QT is one of the most reliable ECG predictors of imminent malignant ventricular dysrhythmia or sudden cardiac death. Expect deterioration within minutes, not hours.
- Do not send unstable or “pre-torsade” patients to CT (even when cerebral T waves are suspected) until the dysrhythmia risk is addressed.
- Overdrive therapy is effective: isoproterenol is ideal; epinephrine or dopamine can be used if iso is unavailable; or use mechanical overdrive pacing.
- Target a heart rate around 120 bpm to shorten the QT interval and suppress torsade.
- Always correct electrolytes immediately: check and aggressively treat hypomagnesemia, hypokalemia, and hypocalcemia.
- The computer will not identify T wave alternans. Recognition is entirely dependent on clinician interpretation.
- R-on-T complexes and mis-sensed pacer spikes on T waves can precipitate torsade or VF. Always confirm your pacer is sensing the QRS, not the T wave.
- A prolonged QT without alternans is common. A prolonged QT with alternans is dangerous.
- Respect the T wave! The T wave carries far more information than clinicians generally appreciate. Morphology, amplitude, and pattern changes often provide critical diagnostic clues.