Recent University of Maryland Medical Center Cases (Part I)
UMEM Potpourri ECG Cases with Dr. Amal Mattu
HPI
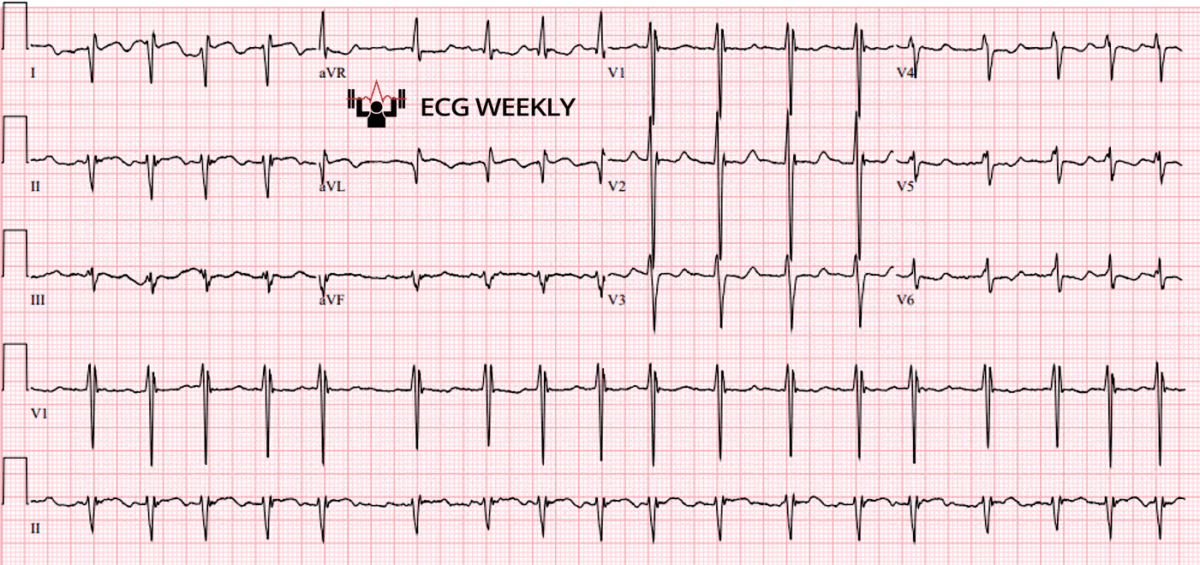
A 67-year-old man presents to the emergency department with chest pain and palpitations. The following ECG is obtained on arrival:
Before watching this week’s workout, carefully review the ECG and consider the following:
-
- What is the axis?
- Would you activate the cath lab for STEMI?
- Would you repeat an ECG?
Video
Kudos
Thanks to the University of Maryland Medical Center's Department of Emergency Medicine for sharing their cases for this series.This week, we’re excited to delve into a series of interesting recent cases from the University of Maryland Medical Center. Each case underscores the importance of a meticulous approach to ECG interpretation and offers valuable lessons for both seasoned clinicians and learners alike. This episode covers five instructive ECG cases, each highlighting critical ECG interpretation pearls and common diagnostic pitfalls.
Case 1: Short QT Interval mimicking STEMI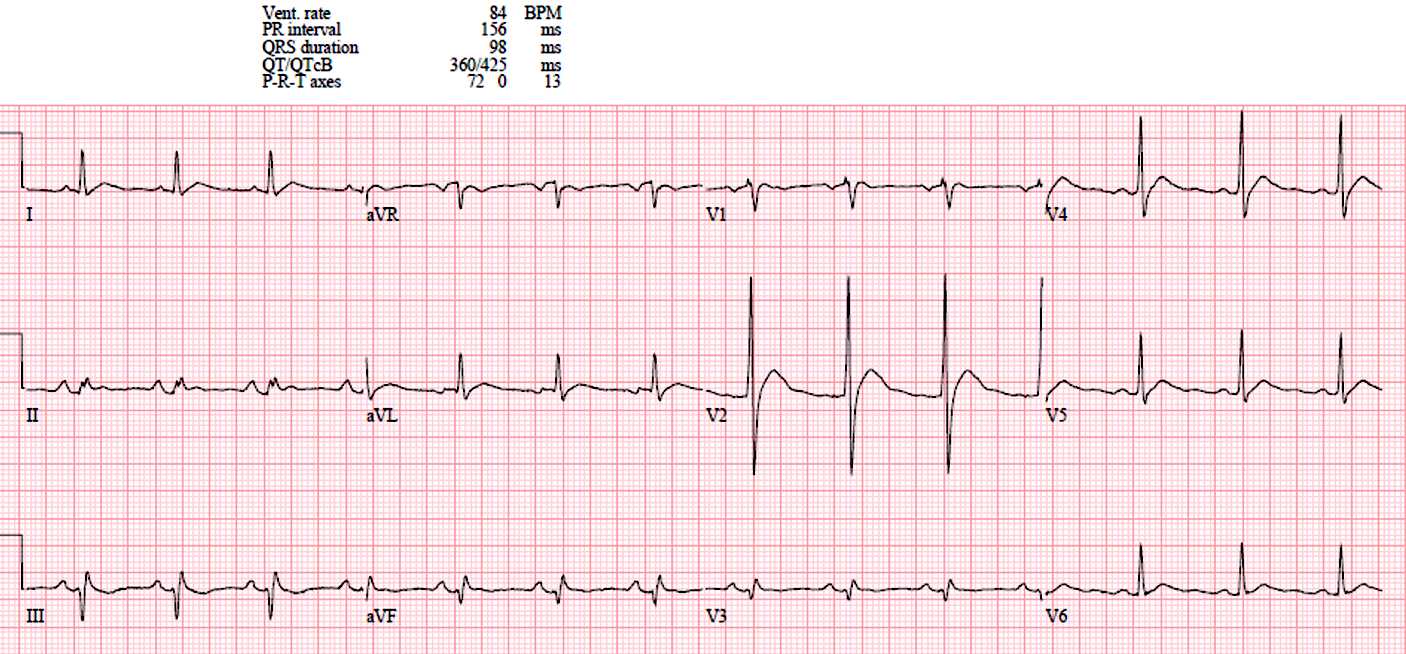
- Patient: 64-year-old man with confusion, malaise, dehydration.
- Key ECG Finding: Short QT interval (QTC in the 300s) with the appearance of ST segment elevation in the anterior leads.
- Diagnosis: Severe hypercalcemia (Calcium: 19.7 mg/dL, Ionized calcium: 2.0 mmol/L) from multiple myeloma.
- Key Points:
- Short QT (especially QTC < 400 ms) strongly suggests hypercalcemia or digoxin effect.
- The shortened QT interval merges the T wave closely with QRS complexes and can mimic STEMI.
Case 2: Baseline artifact and a tricky underlying rhythm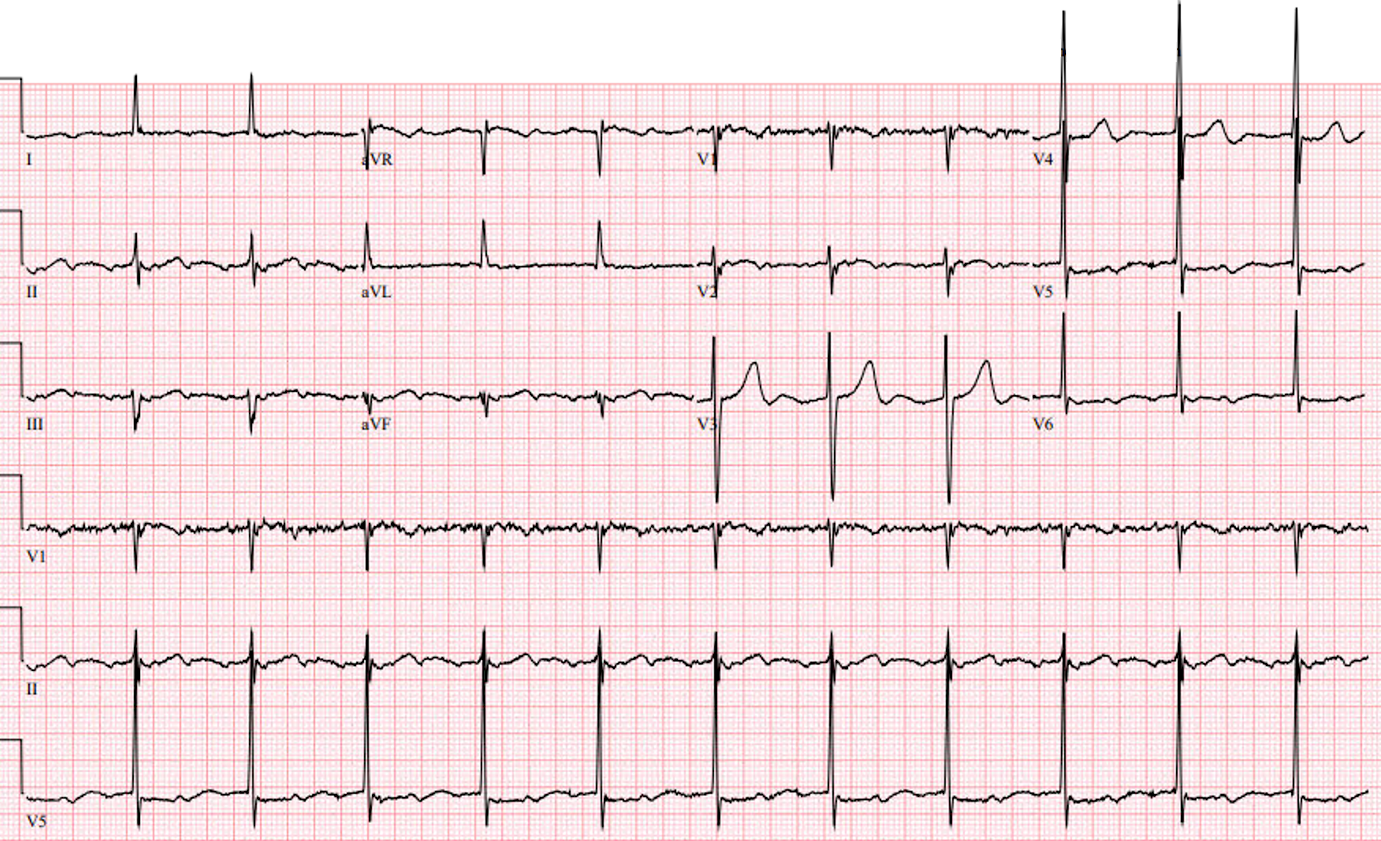
- Patient: 91-year-old man with shortness of breath.
- Key ECG Finding: Atrial flutter initially mistaken for junctional rhythm due to subtle flutter waves (~280-290 bpm) hidden as artifact.
- Diagnosis: Atrial flutter (3:1 conduction).
- Key Points:
- If the heart rate doesn’t change with fluids or movement, suspect atrial flutter or SVT.
- Regular “artifact” that marches out evenly often represents hidden flutter waves. A bumpy baseline might hide P waves.
- Atrial flutter is tricky! Look closely for P waves in all leads.
Case 3: Use of the Bix rule for another tricky rhythm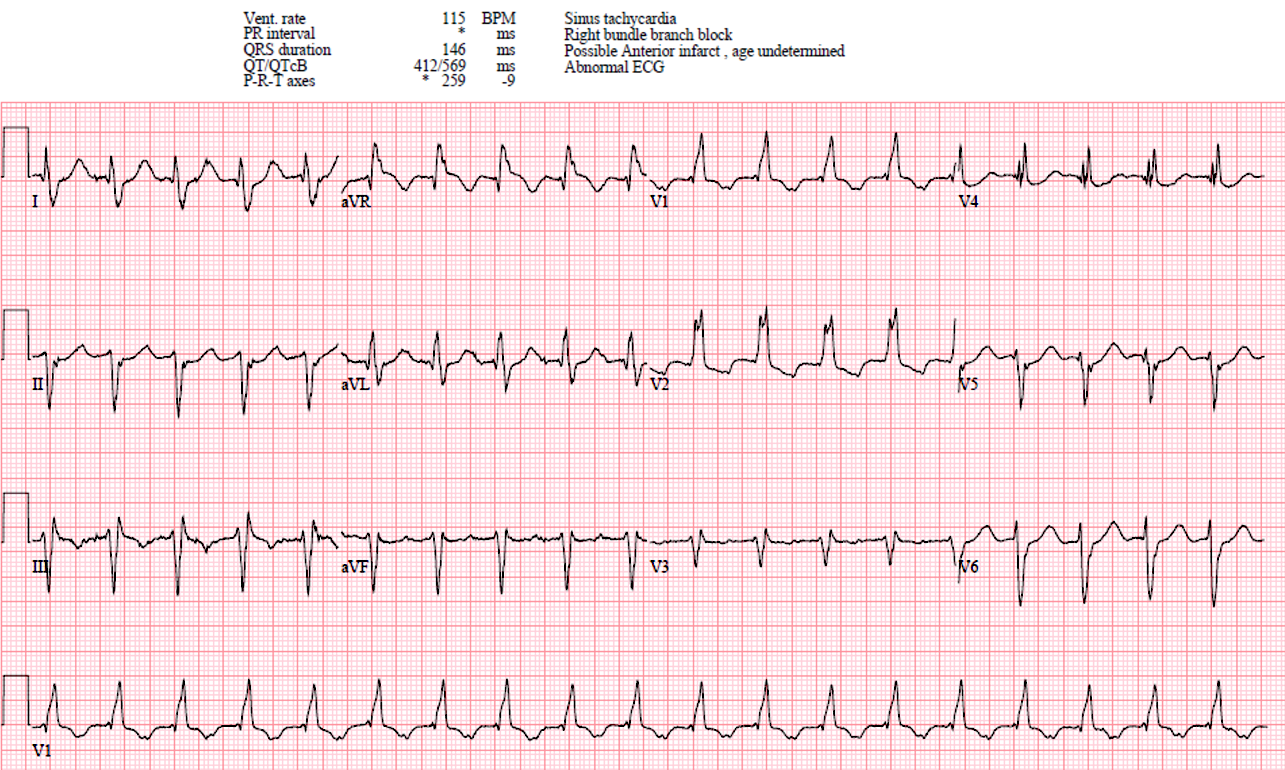
- Patient: 87-year-old woman with chest pain.
- Key ECG Finding: P waves halfway between two QRS complexes (Bix rule), suspicious for atrial flutter. Leads V3 and V4 also seem to be reversed.
- Diagnostic Clarification: Revealed flutter waves with vagal maneuver on repeat ECG.
- Key Points:
- Bix Rule: If a P wave is exactly midway between two QRS complexes, strongly suggests atrial flutter.
- Suspect lead reversal when R wave progression is inconsistent (V3 and V4 were reversed here).
Case 4: Limb lead reversal mimicking STEMI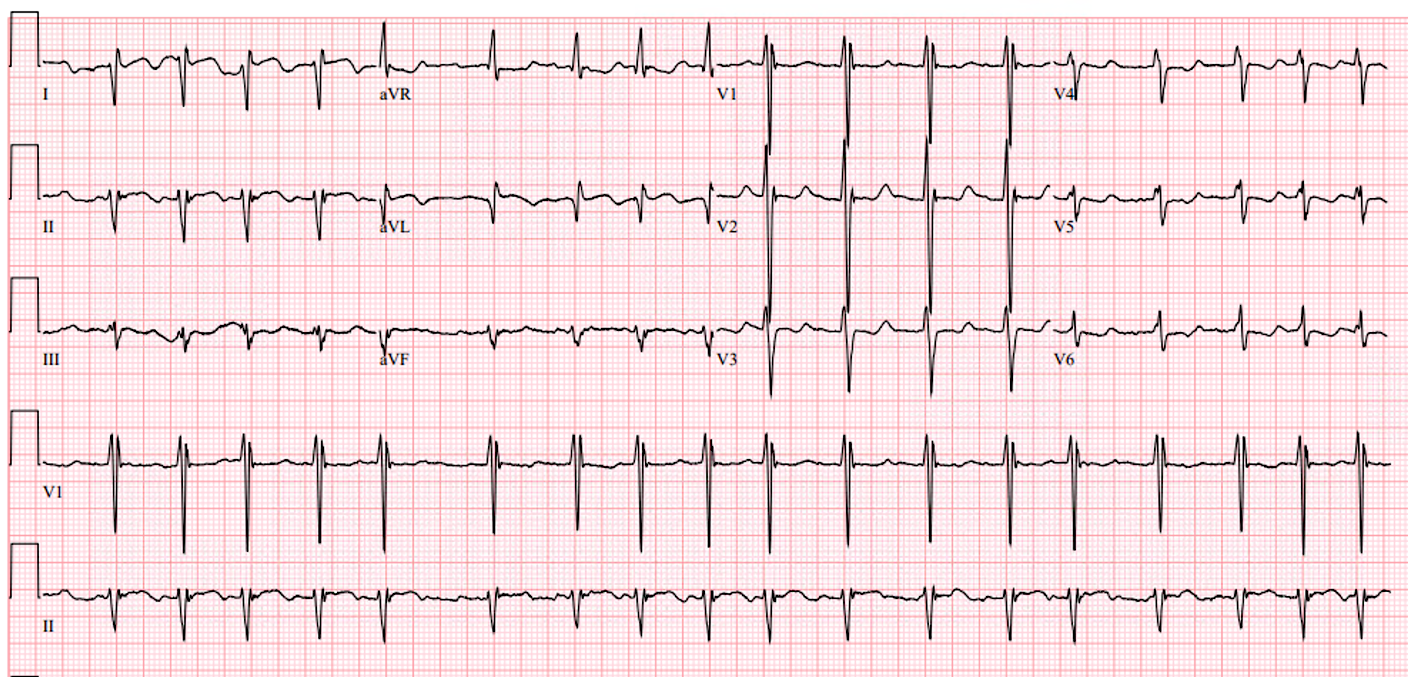
- Patient: 67-year-old man with chest pain and palpitations.
- Initial ECG Finding: Acute high lateral STEMI (ST elevation in I, aVL), however extreme axis deviation is noted which is strange.
- Actual Problem: Limb lead reversal (left arm/right arm leads swapped).
- Corrected lead placement on repeat ECG: Revealed ischemia without STEMI.
- Key Points:
- The QRS axis in I and V6 are usually similar…if they are opposite, consider lead reversal. Extreme axis deviation and discordance between lead I and V6 strongly suggests limb lead reversal.
- Confirming lead placement can prevent incorrect STEMI diagnoses and inappropriate interventions. When the limb lead QRS axes don’t make sense, check the leads!
Case 5: PACs Mistaken for Mobitz II AV Block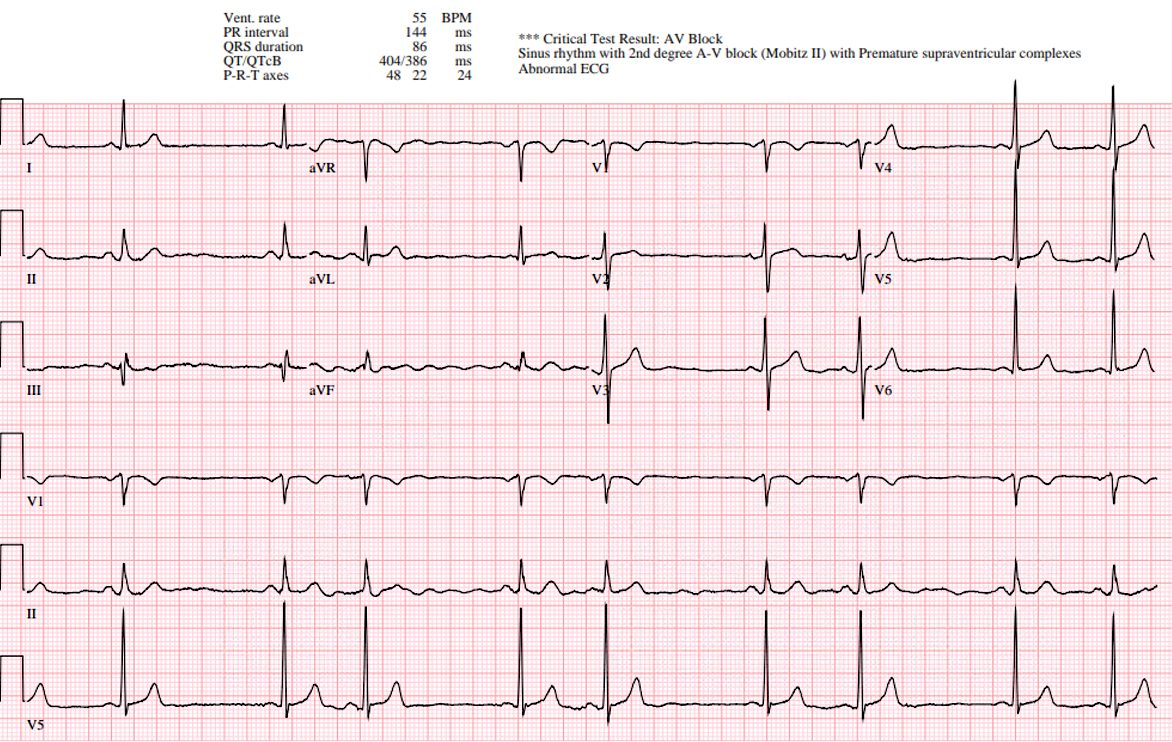
- Patient: 63-year-old man with chest pain.
- Initial Computer Interpretation: Mobitz type II AV block.
- Actual ECG Interpretation: Sinus rhythm with atrial bigeminy (frequent PACs).
- Key Points:
- True Mobitz requires clear, lonely, non-conducted P waves. If there aren’t any lonely P waves, it’s not an AV block!
- Computer commonly misinterprets PAC induced pauses as Mobitz II; always verify manually.
Final Take Home Points:
- Always apply a structured ECG analysis: rate, rhythm, axis, intervals, ischemia.
- Beware of hidden flutter waves and regularly marching artifact.
- Check for limb lead reversal with unusual axis deviations or contradictory leads.
- Do not rely solely on computer interpretations, especially for Mobitz-type blocks.
This week Dr. Mattu emphasized practical ECG reading strategies, reinforcing vigilance against common pitfalls to prevent diagnostic errors and inappropriate treatments. We continue next week with more interesting cases from the University of Maryland ED, stay tuned!