Unrecognized Killers in Emergency Electrocardiography, Part II
ECG Weekly Workout with Dr. Amal Mattu
HPI
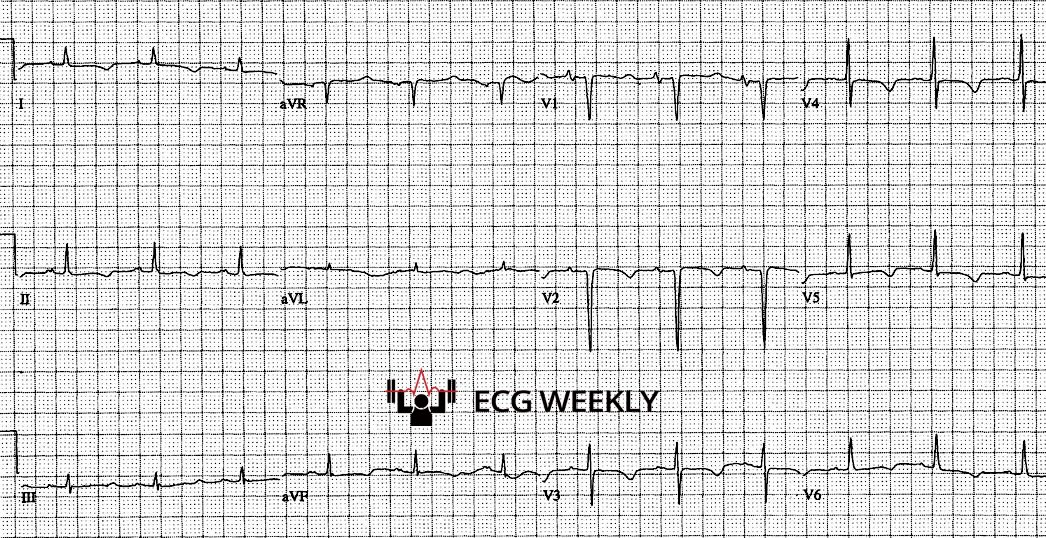
A 46-year-old woman presents after two syncopal episodes associated with palpitations. She reports feeling a rapid heart rate before losing consciousness. She has a few witnessed episodes in the emergency department and is noted to have brief episodes of polymorphic VT that result in syncope but self terminate. The following ECG is obtained between episodes:
Before watching this week’s workout, carefully review the ECG and consider the following:
-
- What is your ECG interpretation and the most likely cause of this patient’s symptoms?
- She is suspected of having Torsades de Pointes and is treated with multiple bolus doses of IV magnesium, but continues to have recurrent syncope and episodes of polymorphic VT. How would you manage this patient?
Video
In this week’s ECG Weekly episode, Dr. Amal Mattu continues his series on Unrecognized Killers in Emergency Electrocardiography, focusing on prolonged QTc intervals and polymorphic ventricular tachycardia. This is part two of a three-part series based on his recent lecture at the UMEM Emergency Cardiology Symposium. You can view the recorded lectures from the recent symposium here.
Main case summary: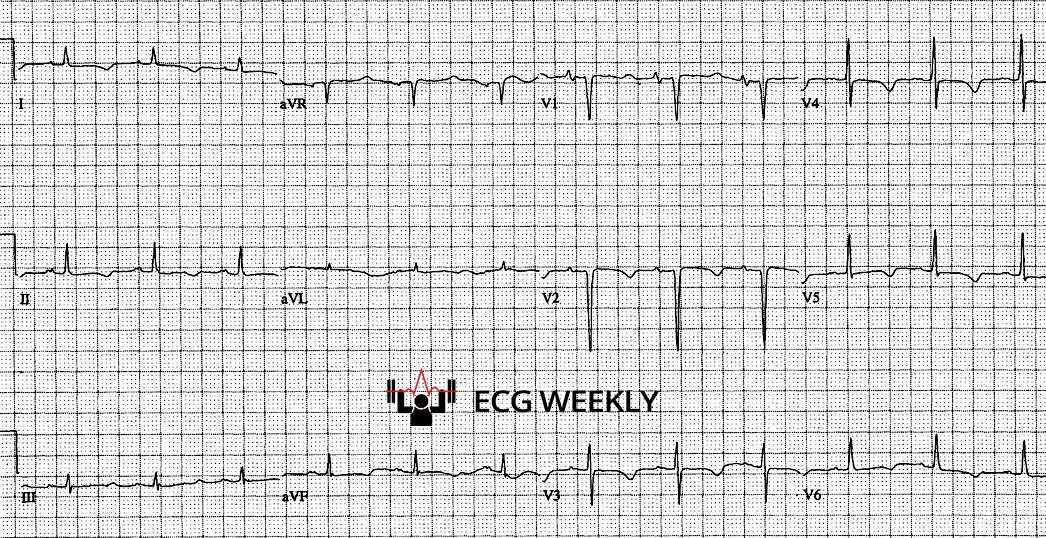
- Patient: A 46-year-old woman with recurrent syncope and documented brief runs of polymorphic ventricular tachycardia.
- ECG between episodes: Prolonged QTc interval due to a long ST segment with normal sized T waves.
- Initial management: Treated with 6 g of IV magnesium (three boluses), which failed to suppress the arrhythmia and led to adverse effects (hypotension, nausea, diaphoresis).
- Correct diagnosis: Hypocalcemia induced QT prolongation, requiring IV calcium, not magnesium.
Key Teaching Points Summary
- Polymorphic VT Must Be Categorized
- Two main types exist:
- Normal QTc: Generic polymorphic VT, most commonly caused by acute ischemia/ACS.
- Prolonged QTc: Torsades de Pointes (TdP), this is diagnosed in sinus rhythm after spontaneous termination or cardioversion.
- Management depends on pre or post event QTc assessment.
- QTc Correction & Interpretation
- The QT interval is corrected for heart rate (QTc) to guide accurate diagnosis and treatment decisions.
- Computer automated QTc measurements made by the ECG machine are generally good at screening but can be unreliable and should not be blindly trusted.
- Overestimate QTc at high heart rate
- Underestimate QTc at low heart rate
- Susceptible to errors in detecting where the QRS starts or where the T wave actually ends (i.e., when U waves, T/U wave fusion, or low amplitude T waves are present).
- The most widely used method for calculating the QTc is the Bazett’s formula: QTc = QT / √ RR
- QT and RR are measured in seconds (e.g., QT = 0.44 s, RR = 0.8 s).
- Alternative standard correction formulas exist (Fridericia’s, Framingham, and Hodges formulas), but no single correction method is definitively superior to others.
- A quick visual estimation method known as the “Quick QTc or Half the RR Interval Rule” suggests that if the T wave ends before the halfway mark between two R waves, then the QTc is not significantly prolonged (< 500 ms). While this method is quick and convenient, it also has limitations at heart rate extremes. Precise evaluation requires formal correction formulas and manual measurements.
- QTc > 500 ms is High Risk for Torsades
- Always investigate for underlying causes when QTc ≥ 500 ms.
- Differential Diagnosis for Prolonged QTc
- Electrolyte Abnormalities:
- Hypokalemia (due to U waves)
- Hypomagnesemia
- Hypocalcemia (specifically prolongs the ST segment, not T wave)
- Many Medications: Sodium channel blockers, methadone, certain psychiatric medications, etc.
- Miscellaneous:
- Elevated intracranial pressure
- Hypothermia (also diagnosed using a thermometer)
- Congenital long QT syndromes
- Electrolyte Abnormalities:
- Differentiate the QT Prolongation Source
- Long ST segment with normal T waves = think hypocalcemia.
- Stretched T wave / TU fusion = think hypokalemia or hypomagnesemia.
- This distinction determines the most appropriate treatment: calcium vs. magnesium.
- Magnesium Is Not Always the Answer
- Magnesium is the first-line treatment for TdP due to prolonged QT, but is usually most helpful in T wave related QT prolongation (e.g., hypokalemia or hypomagnesemia).
- If the ST segment is specifically prolonged (e.g., hypocalcemia), magnesium is not likely to help, and calcium is the most appropriate treatment.
- Practice-Changing Tips from Dr. Mattu
- In patients with suspected severe dehydration or electrolyte derangement (e.g., severe gastroenteritis or alcohol withdrawal), obtain a screening 12-lead ECG to evaluate the QTc.
- If QTc is prolonged, place the patient on cardiac monitoring while labs are pending to detect and intervene on TdP early.
- Dr. Mattu shares three cases in this episode where this approach led to life-saving interventions.
7. Clinical Pearls for QTc Management
- QTc Threshold: > 500 ms is high risk for TdP. Shorter intervals are < 500 ms are less concerning, though not completely risk-free.
- Identify and treat the underlying cause promptly (electrolytes, medication-induced QT prolongation, etc.).
- For acquired causes of prolonged QT:
- Avoid bradycardia which will further lengthen the QT (beta-blockers are contraindicated in acquired cases).
- Hold offending medications and avoid any new QT prolonging medications (avoid amiodarone and procainamide).
- Speed up the heart rate (target 100-120 bpm) using isoproterenol, dopamine, epinephrine, or overdrive mechanical pacing.
- Magnesium sulfate: Use for TdP unless QT prolongation is due specifically to hypocalcemia.
- If TdP is persistent or unstable, immediate defibrillation is required.
Bottom Line:
-
- If you are really worried about someone’s electrolytes (e.g., severe dehydration or suspected electrolyte derangement), get a STAT ECG and check the QTc while waiting on lab results!
- If QTc ≥ 500 ms, place the patient on a cardiac monitor (avoid hallways or non-monitored areas) and correct the underlying cause whenever possible.
- Recognize that magnesium is not always the answer; if the QTc is prolonged specifically because of a long ST segment (as opposed to a large or abnormal T wave), think hypocalcemia and treat with calcium.
- An early ECG can predict electrolyte emergencies and save lives before labs result.