Key Points:
- An ECG records voltage differences over time. The ECG tracing is a plot where the horizontal axis is time and the vertical axis is voltage.
- Leads are viewpoints. Each lead displays the projection of the heart’s net electrical vector onto that lead’s axis.
- Direction matters as much as magnitude. A wavefront moving toward a lead’s positive pole produces an upward deflection; moving away produces a downward deflection.
- Normal activation follows a predictable sequence (SA node to atria to AV node to His-Purkinje to ventricles). Understanding the sequence explains most ECG morphology before memorization.
- Lead placement errors and technical factors are common causes of false diagnoses. When an ECG looks “impossible,” verify the setup.

1) What the ECG Measures
An ECG does not measure “electricity in the heart” directly. It measures voltage differences at the skin created by cardiac depolarization and repolarization. The display is a time-voltage graph:
- Time: left to right (paper speed typically 25 mm/s)
- Voltage: up and down (calibration typically 10 mm/mV)
Standard calibration reminders:
- At 25 mm/s: small box 40 ms, large box 200 ms
- At 10 mm/mV: 10 mm vertical deflection equals 1 mV
Dive deeper here:
2) Vectors: the single idea that explains most ECG patterns
During depolarization and repolarization, the heart generates a net electrical vector at any instant. Each ECG lead shows the component of that vector along the lead’s axis.
Practical rules:
- Vector toward the lead’s positive pole results in an upward deflection.
- Vector away from the positive pole results in a downward deflection.
- Vector perpendicular to the lead axis produces a small deflection or a biphasic complex.
- Larger vectors (more myocardium participating or more synchronized activation) generally produce larger amplitudes, but electrode position and body habitus matter.
This is why the same rhythm can look different across leads. Nothing magical is happening. You are simply rotating viewpoints using the different leads.
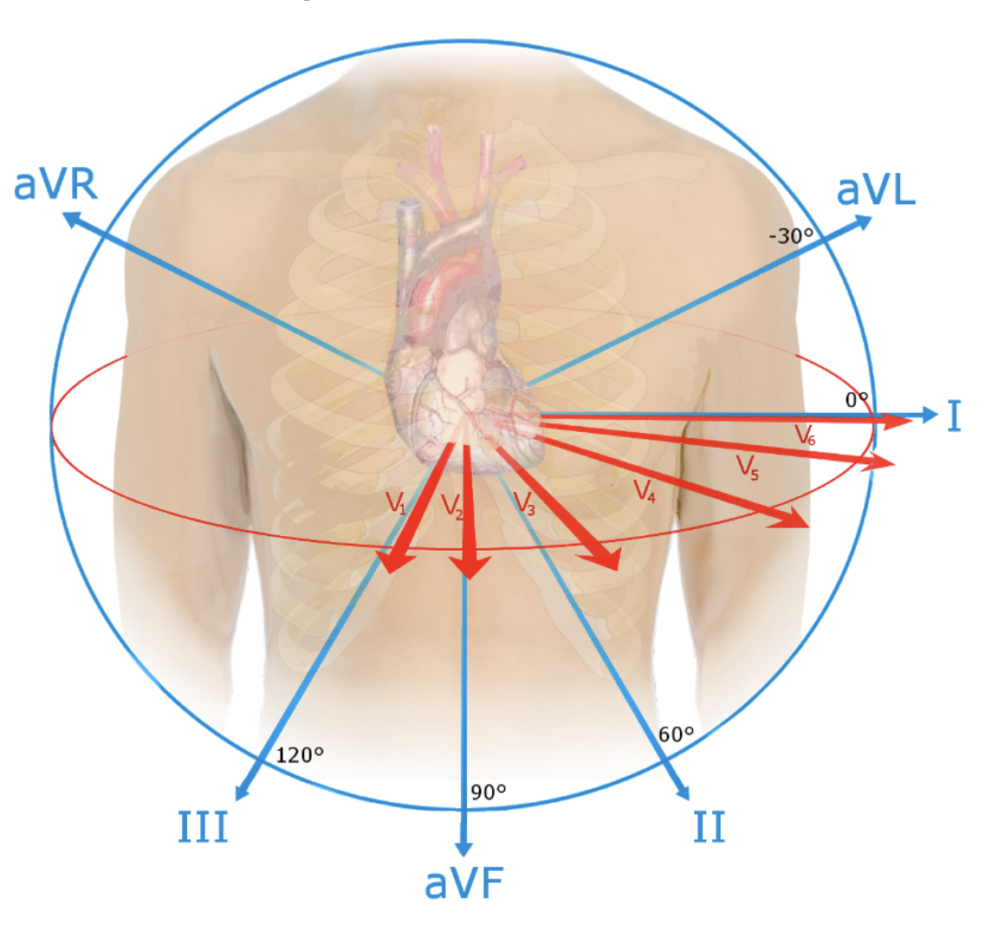
3) Leads: viewpoints in two planes
The standard 12-lead ECG provides multiple “camera angles” on the same event.
Frontal plane (limb leads)
- Leads I, II, III, aVR, aVL, aVF
- These view the heart from the front and define the frontal plane axis.
Horizontal plane (precordial leads)
- Leads V1–V6
- These view the heart from the chest and define the horizontal plane progression (including R-wave progression).
Key concept:
- Each lead’s tracing is the projection of the same activation wavefront onto that lead’s axis. Differences across leads are expected and informative
Learn more about voltage and axis here:
4) Activation: normal conduction and what it creates on the ECG
The ECG waveform sequence is not arbitrary. It is the surface reflection of a predictable activation pattern.
Normal conduction pathway
SA node → atria → AV node → His bundle → right and left bundle branches → Purkinje system → ventricles
What that sequence explains:
- P wave: atrial depolarization
- PR segment/interval: AV nodal delay and conduction through the His-Purkinje system up to ventricular activation
- QRS: ventricular depolarization (rapid because His-Purkinje activation is fast and synchronized)
- ST segment: early repolarization phase when ventricles are relatively electrically uniform
- T wave: ventricular repolarization
Learn more about normal conduction here:
5) Lead placement: why it matters
Because leads are viewpoints, incorrect placement changes the viewpoint and can create patterns that mimic pathology.
Common consequences:
- Altered axis and QRS polarity
- Abnormal R-wave progression
- False ST elevation or depression
- Apparent infarct patterns that disappear when leads are corrected
Practical habit:
- If you see an ECG that is discordant with the clinical story or appears internally inconsistent (axis, progression, territories), consider misplacement and repeat the ECG with verified placement.
Learn more about lead placement here:
Key Clinical Pearls:
- Treat the ECG as a vector projection tool. When you understand the lead axis, morphology becomes explainable rather than memorized.
- “Weird ECGs” are often weird viewpoints. Verify calibration, artifact, and lead placement before calling a rare diagnosis.
- Conduction sequence predicts morphology. When the pattern breaks the rules, ask: is this conduction disease, ectopy, pre-excitation, pacing, or misplacement?
- Systematic Approach: Always use a consistent, step-by-step approach to ECG interpretation to ensure that no important findings are overlooked.
- Correlate with Clinical Context: ECG findings should always be interpreted in light of the patient’s symptoms and clinical history for accurate diagnosis and treatment.
- Recognize Normal Variants: Familiarize yourself with normal variants to avoid over-diagnosing conditions based on benign ECG findings.
Explore related content:


