Key Points for EMS Providers:
You are the first critical link in the chain of survival for ACS patients—your actions set the course for their care, directly impacting time to treatment and survival. The decisions you make, from rapid ECG acquisition to early STEMI activation, saves valuable time and can save lives. Here are ten key points to consider:
- A 12-lead ECG should be obtained within 10 minutes of first medical contact (FMC)—early STEMI recognition shaves critical minutes off door-to-balloon time.
- ECG transmission to the receiving hospital is a game-changer—prehospital activation of the cath lab can significantly reduce delays and improve survival.
- Always provide a physical or electronic copy of your ECG to the hospital team—early ECGs may reveal ischemic changes that resolve before hospital arrival, making them diagnostic and critical for decision-making.
- Serial ECGs can catch evolving STEMIs—if the first ECG is non-diagnostic but suspicion is high, repeat it.
- Right-sided and posterior ECGs may be necessary to detect STEMI and equivalent patterns, such as right ventricular infarction or posterior MI.
- ACS can present with subtle findings or an initially normal ECG—clinical judgment is crucial. STEMI and STEMI equivalent patterns are managed similarly, but lack of these criteria does not rule out ACS.
- EMS transport directly to PCI-capable centers is preferred for STEMI, aiming for an FMC-to-device time ≤ 90 minutes.
- Limb lead misplacement, artifact, and poor electrode contact can mimic pathology—double-check placement before activating a cath lab.
- Beware STEMI imposters! Conditions like pericarditis, LVH, and hyperkalemia can mimic STEMI—correlate ECG findings with clinical context. All ACS patients should have clinical symptoms of acute cardiac ischemia.
- In cases of cardiac arrest, immediate rhythm analysis and ECG acquistion post-ROSC are critical for guiding reperfusion decisions.
EMS as the First Line in STEMI Care
- Rapid recognition and transmission of STEMI & STEMI equivalent ECG patterns kickstart the entire ACS response.
- A prehospital ECG may be the only one showing diagnostic changes—ischemic findings can normalize by the time the patient arrives, leading to missed STEMIs if EMS ECGs are not reviewed.
- Decision to transport directly to a PCI center can be the difference between life and death.
- EMS communication with ED and cardiology teams ensures seamless STEMI activation—every second matters.
EMS ECG Best Practices (from the 2025 ACC/AHA/ACEP ACS Guidelines)
1. Obtain a Focused History/Physical Exam & at Least One High-Quality 12-Lead ECG
- Patients with suspected ACS should be transported to the ED by EMS rather than by private vehicle. After obtaining a focused history and physical exam (with assessment of vital signs), obtain at least one 12-lead ECG to facilitate next steps in patient triage.
- Timing: Perform within 10 minutes of first medical contact (FMC). Early acquisition is associated with shorter reperfusion times and lower mortality.
- Management: Based on presence or absence of ST segment elevation (or suspected equivalent). Trained EMS personnel have been shown to be able to interpret STEMI ECGs with high accuracy.
- Placement: Ensure correct lead positioning—limb lead misplacement or poor electrode contact can mimic signs of ischemia and cause other ECG abnormalities that may lead to confusion.
- No STEMI but high clinical suspicion? Repeat the ECG, especially if symptoms persist or clinical condition deteriorates.
- 11 % of patients ultimately diagnosed with STEMI had an initial ECG that was non-diagnostic. 72% of those has a follow up ECG that was diagnostic of STEMI within 90 minutes. However, serial ECGs should not delay transport to the hospital.
- A second or third ECG may identify up to 15% of additional STEMI cases not present on the first ECG. In one study, a STEMI diagnosis was made in an extra 8% of patients within 12 minutes of the first nondiagnostic ECG. Repeating an ECG when appropriate can change and improve care.
- ACS with a normal initial ECG does not rule out acute ischemia. ECG changes are not required to diagnose ACS.
2. Transmit STEMI ECGs & Bring Copies of All Prehospital ECGs Obtained
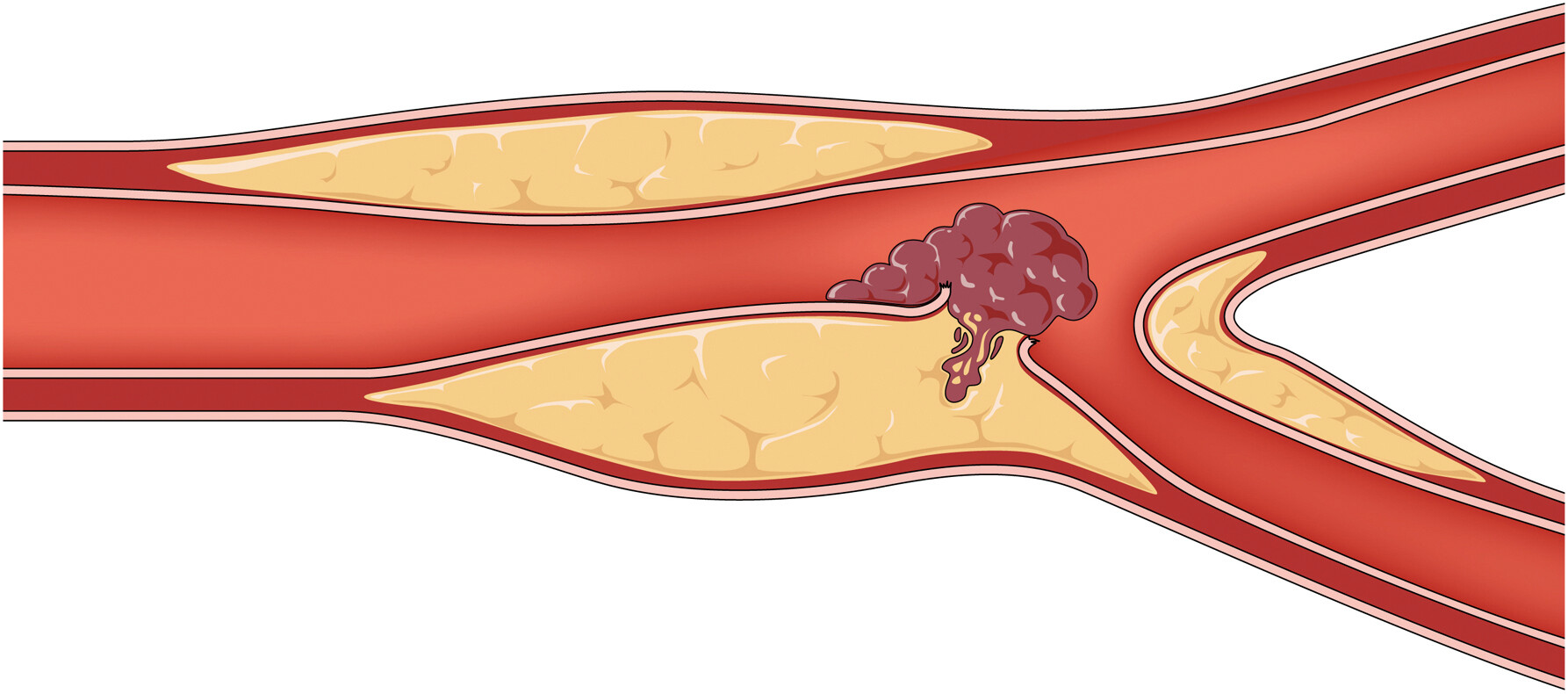
- Prehospital ECG transmission enables early STEMI activation, reducing door-to-balloon time.
- Rapid reperfusion is associated with improved myocardial salvage and survival.
- Each 30 mins of delay is associated with increase in relative risk of 1-year mortality by 7.5%.
- Prehospital STEMI or equivalent patterns should be transported to PCI capable hospitals with goal of FMC to device time of ≤ 90 minutes.
- Always provide a printed or electronic copy to the ED team—subsequent ECGs may miss transient ST changes that were present on initial or early recordings. Making sure the accepting team is aware of all important events and prehospital findings makes a difference.
3. Identify STEMI & Equivalent ECG Patterns
- STEMI Identification Criteria:
- New or presumed new ST segment elevation of ≥1 mm in two or more anatomically contiguous leads (measured at the J-point) in all leads except in V2-V3 (where age/sex-specific criteria apply):
- ≥ 2 mm in men ≥ 40 years old
- ≥ 2.5 mm in men < 40 years old
- ≥ 1.5 mm in women regardless of age
- New or presumed new LBBB should not automatically be a considered STEMI-equivalent unless the patient is unstable or has Sgarbossa criteria.
- Posterior Leads (V7-V9)
- Indicated for isolated ST depression in V1-V3 to rule out posterior STEMI.
- Right-Sided Leads (V4R-V6R)
- Used in patients with inferior STEMI to assess for right ventricular infarction, which may alter management (avoidance of nitroglycerin).
- Used in patients with inferior STEMI to assess for right ventricular infarction, which may alter management (avoidance of nitroglycerin).
- New or presumed new ST segment elevation of ≥1 mm in two or more anatomically contiguous leads (measured at the J-point) in all leads except in V2-V3 (where age/sex-specific criteria apply):
4. Beware of Cardiogenic Shock & STEMI Mimics
- Early recognition of cardiogenic shock in ACS patients is key to initial triage and risk stratification.
- Cardiogenic shock related to acute MI is present in ~ 7-10% of the ACS population and carries a high mortality rate. Recognising signs of acute heart failure and shock associated with ACS can help the accepting team prepare.
- There are more than 15 other causes of ST segment elevation aside from STEMI. Common causes of false STEMI activations:
- Hyperkalemia (peaked T waves, wide QRS)
- Pericarditis (diffuse ST elevation, no reciprocal changes)
- LVH or BBB (baseline ST/T abnormalities)
- Check for lead misplacement if the ECG doesn’t match the clinical picture.
5. Know Your Local STEMI/Cardiac Arrest Transport Protocols
- Direct transport to a PCI-capable center is the goal.
- FMC-to-balloon time should be ≤ 90 minutes.
- If PCI is not available within 120 minutes, consider fibrinolytics if there are no contraindications.
- ~10% of STEMI patients transferred by EMS are estimated to have an out-of-hospital cardiac arrest. Survival-to-hospital discharge in the patient who is comatose with out-of-hospital cardiac arrest is < 10% regardless of the cause.
- Those with witnessed arrest and shockable rhythm have improved survival.
- Outcomes for STEMI patients who are awake after resuscitated cardiac arrest are comparable to STEMI patients who did not have cardiac arrest. Hence, awake post-arrest STEMI patients are candidates for PCI.
- Patients with cardiac arrest and STEMI who are non-comatose or comatose with favorable prognostic features, should undergo PCI to improve survival.
- Those who are comatose and have unfavorable prognostic features (unwitnessed arrest, no bystander CPR, nonshockable rhythm, CPR > 30 minutes, time to ROSC > 30 mins, arterial pH < 7.2, lactate > 7 mmol/L, age > 85 years, end stage renal disease on dialysis), may sometimes undergo PCI after further individualized assessment.
- In patients who are comatose, electrically/hemodynamically stable, and do NOT have evidence of STEMI, immediate angiography is not recommended due to lack of benefit.
Key Clinical Pearls for EMS:
- EMS providers are the first link in the ACS survival chain—your ECG and actions dictate the next steps in patient care.
- Transmitting the ECG can save lives—early cath lab activation speeds up revascularization.
- Prehospital ECG may be diagnostic even if the hospital ECG is normal—bring a copy and emphasize its importance.
- Serial ECGs matter—if symptoms persist and the first ECG is normal, repeat it so long as it does not delay transport.
- When in doubt, treat as STEMI and transport accordingly—early intervention saves lives.
- EMS doesn’t just transport patients—you are the front line in diagnosing and initiating life-saving care for STEMI. Your rapid ECG interpretation, transmission, and documentation are critical to reducing morbidity and mortality. Keep doing what you do best—saving lives, one ECG at a time.
Learn more about early ACS and ECG evidence of acute coronary occlusion MI:
Most Recent US & European ACS Guidelines:
- Rao, S, O’Donoghue, M, Ruel, M. et al. 2025 ACC/AHA/ACEP/NAEMSP/SCAI Guideline for the Management of Patients With Acute Coronary Syndromes: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. JACC. Feb 27, 2025. PMID: 40014670
- Zoni CR, Mukherjee D, Gulati M. Proposed new classification for acute coronary syndrome: Acute coronary syndrome requiring immediate reperfusion. Catheter Cardiovasc Interv. 2023 Jun;101(7):1177-1181. Epub 2023 Apr 16. PMID: 37061867
- Byrne RA, Rossello X, Coughlan JJ, et al; ESC Scientific Document Group. 2023 ESC Guidelines for the management of acute coronary syndromes. Eur Heart J. 2023 Oct 12;44(38):3720-3826. PMID: 37622654
- Supplementary Data for the 2023 ESC Guidelines for the management of acute coronary syndromes. Full text link
- Kontos MC, de Lemos JA, Deitelzweig SB, et al. 2022 ACC Expert Consensus Decision Pathway on the Evaluation and Disposition of Acute Chest Pain in the Emergency Department: A Report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2022 Nov 15;80(20):1925-1960. PMID: 36241466
- Writing Committee Members, Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the Evaluation and Diagnosis of Chest Pain: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2021 Nov 30;78(22):e187-e285. Epub 2021 Oct 28. PMID: 34756653
- Thygesen K, Alpert JS, Jaffe AS, et al. Fourth Universal Definition of Myocardial Infarction (2018). J Am Coll Cardiol 2018;72(18):2231-64. PMID: 30153967
- Writing Committee Members, Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI Guideline for Coronary Artery Revascularization: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2021 Dec 7:S0735-1097(21)06158-1. Epub ahead of print. PMID: 34895950
- Dehmer GJ, Badhwar V, Bermudez EA, et al. 2020 AHA/ACC Key Data Elements and Definitions for Coronary Revascularization: A Report of the ACC/AHA Task Force on Clinical Data Standards (Writing Committee to Develop Clinical Data Standards for Coronary Revascularization). J Am Coll Cardiol. 2020 Apr 28;75(16):1975-2088. Epub 2020 Mar 23. PMID: 32217040
- Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J 2017;39(2):119-77. PMID: 28886621
- Amsterdam EA, Wenger NK, Brindis RG, et al. ACC/AHA Task Force Members. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014 Dec 23;130(25):e344-426. PMID: 25249585
- O'Gara PT, Kushner FG, Ascheim DD, at al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013 Jan 29;61(4):e78-e140. PMID: 23256914
Recommended Reading on OMI vs. STEMI Paradigm Shift:
- Ricci F, Martini C, Scordo DM, et al. ECG Patterns of Occlusion Myocardial Infarction: A Narrative Review. Ann Emerg Med. 2025 Jan 17:S0196-0644(24)01250-2. PMID: 39818676.
- McLaren JTT, de Alcanar JN, Aslanger EK, et al. From ST-Segment Elevation MI to Occlusion MI: The New Paradigm Shift in Acute Myocardial Infarction. JACC: Advances, Vol 3, Issue 11. Epub 2024 Nov. Full text link.
- McLaren JTT, El-Baba M, Sivashanmugathas V, Meyers HP, Smith SW, Chartier LB. Missing occlusions: Quality gaps for ED patients with occlusion MI. Am J Emerg Med. 2023 Nov;73:47-54. Epub 2023 Aug 15. PMID: 37611526
- Smith SW, Meyers HP. Hyperacute T-waves Can Be a Useful Sign of Occlusion Myocardial Infarction if Appropriately Defined. Ann Emerg Med. 2023 Aug;82(2):203-206. Epub 2023 Mar 3. PMID: 36872197
- Spirito A, Vaisnora L, Papadis A, et al. Acute Coronary Occlusion in Patients With Non-ST-Segment Elevation Out-of-Hospital Cardiac Arrest. J Am Coll Cardiol. 2023 Feb 7;81(5):446-456. PMID: 36725173
- Avdikos G, Michas G, Smith SW. From Q/Non-Q Myocardial Infarction to STEMI/NSTEMI: Why It's Time to Consider Another Simplified Dichotomy; a Narrative Literature Review. Arch Acad Emerg Med. 2022 Oct 1;10(1):e78. PMID: 36426169
- Al-Zaiti S, Macleod R, Dam PV, et al. Emerging ECG methods for acute coronary syndrome detection: Recommendations & future opportunities. J Electrocardiol. 2022 Sep-Oct;74:65-72. Epub 2022 Aug 18. PMID: 36027675
- Xu C, Melendez A, Nguyen T, et al. Point-of-care ultrasound may expedite diagnosis and revascularization of occult occlusive myocardial infarction. Am J Emerg Med. 2022 Aug;58:186-191. Epub 2022 Jun 8. PMID: 35700615
- McLaren JTT, Meyers HP, Smith SW, et al. From STEMI to occlusion MI: paradigm shift and ED quality improvement. CJEM. 2021 Dec 30. Epub PMID: 34967919
- Meyers HP, Bracey A, Lee D, et al. Accuracy of OMI ECG findings versus STEMI criteria for diagnosis of acute coronary occlusion myocardial infarction. Int J Cardiol Heart Vasc. 2021 Apr 12;33:100767. PMID: 33912650
- Aslanger EK, Meyers HP, Smith SW. Recognizing electrocardiographically subtle occlusion myocardial infarction and differentiating it from mimics: Ten steps to or away from cath lab. Turk Kardiyol Dern Ars. 2021 Sep;49(6):488-500. PMID: 34523597
- Khawaja M, Thakker J, Kherallah R, et al. Diagnosis of Occlusion Myocardial Infarction in Patients with Left Bundle Branch Block and Paced Rhythms. Curr Cardiol Rep. 2021 Nov 17;23(12):187. PMID: 34791609
- Meyers HP, Bracey A, Lee D, et al. Ischemic ST-Segment Depression Maximal in V1-V4 (Versus V5-V6) of Any Amplitude Is Specific for Occlusion Myocardial Infarction (Versus Nonocclusive Ischemia). J Am Heart Assoc. 2021 Dec 7;10(23):e022866. Epub 2021 Nov 15. PMID: 34775811
- Meyers HP, Bracey A, Lee D, et al. Comparison of the ST-Elevation Myocardial Infarction (STEMI) vs. NSTEMI and Occlusion MI (OMI) vs. NOMI Paradigms of Acute MI. J Emerg Med. 2021 Mar;60(3):273-284.Epub 2020 Dec 9. PMID: 33308915
- Aslanger EK, Yıldırımtürk Ö, Şimşek B, et al. DIagnostic accuracy oF electrocardiogram for acute coronary OCClUsion resuLTing in myocardial infarction (DIFOCCULT Study). Int J Cardiol Heart Vasc. 2020 Jul 30;30:100603. PMID: 32775606
- Hillinger P, Strebel I, Abächerli R, et al. APACE Investigators. Prospective validation of current quantitative electrocardiographic criteria for ST-elevation myocardial infarction. Int J Cardiol. 2019 Oct 1;292:1-12. Epub 2019 Apr 11. PMID: 31056411
- Miranda DF, Lobo AS, Walsh B, et al. New Insights Into the Use of the 12-Lead Electrocardiogram for Diagnosing Acute Myocardial Infarction in the Emergency Department. Can J Cardiol. 2018 Feb;34(2):132-145. Epub 2017 Nov 29. PMID: 29407007
Recommended Reading to Learn More About ACS and Ischemic Chest Pain:
- Meyers HP, Smith SW. Acute Coronary Syndromes. In: Mattu A and Swadron S, ed. CorePendium. Burbank, CA: CorePendium, LLC. Accessed January 1, 2024. https://www.emrap.org/corependium/ACSchapter
- Fanaroff AC, Rymer JA, Goldstein SA, et al. Does This Patient With Chest Pain Have Acute Coronary Syndrome?: The Rational Clinical Examination Systematic Review. JAMA. 2015 Nov 10;314(18):1955-65. PMID: 26547467


